Verapamil vs. Blood Pressure Alternatives Comparison Tool
Medication Overview
Verapamil (Isoptin) is a calcium-channel blocker used for hypertension, angina, and certain arrhythmias. It works by blocking calcium channels in the heart and blood vessels, leading to vasodilation and reduced heart rate.
Common side effects include constipation, dizziness, and bradycardia. It's contraindicated in severe heart failure cases.
Monthly Cost: $12-$20 (generic)
Effectiveness
- High Blood Pressure Control
- High Angina Relief
- Moderate Arrhythmia Management
Side Effects Profile
- Constipation Common
- Bradycardia Moderate
- Heart Failure Risk High
- Dizziness Moderate
Key Takeaways
- Isoptin (Verapamil) is a calcium‑channel blocker used for hypertension, angina, and certain arrhythmias.
- Primary alternatives include other calcium‑channel blockers (Diltiazem, Amlodipine), beta‑blockers (Metoprolol, Atenolol) and ACE inhibitors (Lisinopril).
- Verapamil offers strong heart‑rate control but can worsen heart failure; alternatives differ in side‑effect profiles.
- Cost, dosing frequency, and drug interactions often decide which option fits a patient best.
- Switching meds requires a taper plan, monitoring, and a checklist to avoid rebound hypertension.
Isoptin is the brand name for Verapamil, a calcium‑channel blocker that relaxes blood vessels and slows the heart’s conduction system. It’s prescribed for high blood pressure, chronic stable angina, and specific supraventricular tachyarrhythmias.
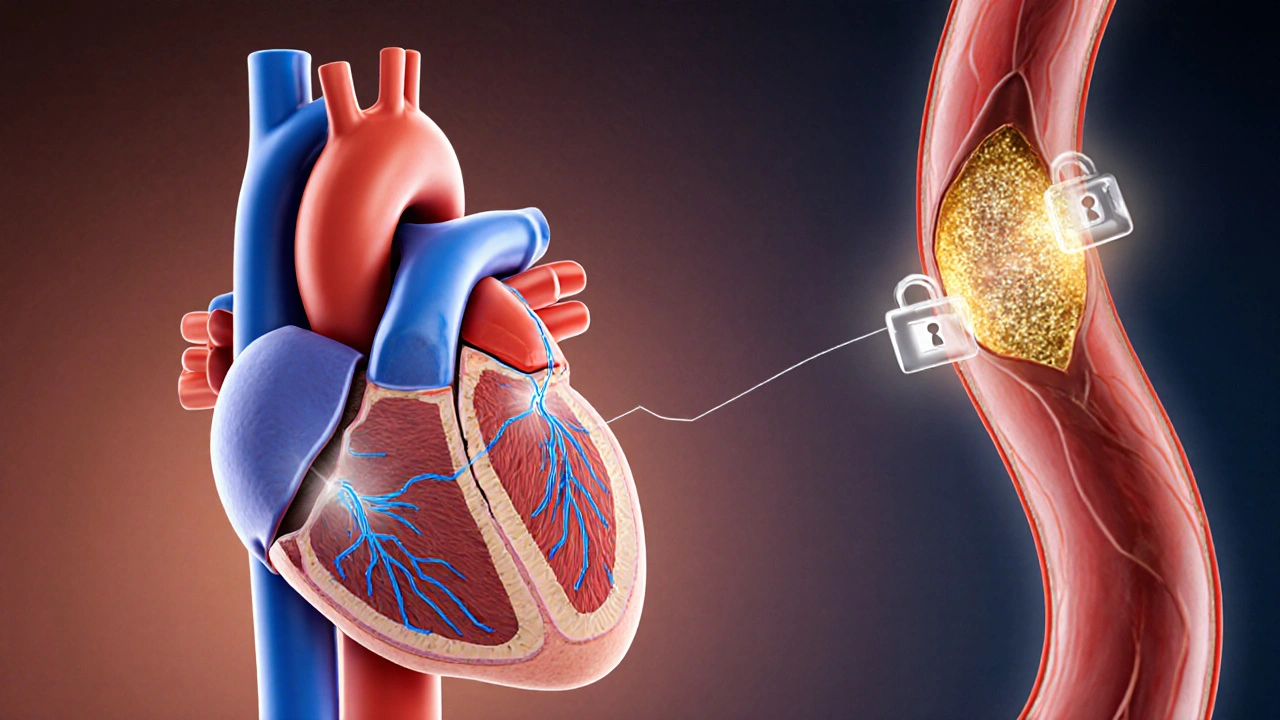
How Verapamil Works
Verapamil blocks L‑type calcium channels in cardiac and vascular smooth muscle. By reducing calcium influx, it lessens contractility, dilates arteries, and slows electrical signals through the AV node. This triple action makes it useful for both blood‑pressure control and rhythm management.
When Doctors Choose Verapamil
Typical indications include:
- Essential hypertension when other first‑line agents are unsuitable.
- Stable angina that persists despite beta‑blockers or nitrates.
- Rate control for atrial fibrillation or flutter, especially when beta‑blockers are contraindicated.
Because it can depress myocardial contractility, clinicians avoid Verapamil in patients with severe left‑ventricular dysfunction (ejection fraction <40%).
Side Effects and Safety Concerns
Common adverse events are:
- Dizziness or light‑headedness from lowered blood pressure.
- Constipation (up to 10% of users).
- Peripheral edema, especially at higher doses.
Serious risks include bradycardia, AV‑block, and worsening heart failure. Drug interactions are notable with:
- CytochromeP450 3A4 inhibitors (e.g., clarithromycin) - raise Verapamil levels.
- Beta‑blockers - may cause excessive heart‑rate slowing.
- Digoxin - increase risk of toxicity.
Top Alternatives to Verapamil
Below are the most frequently considered substitutes, grouped by drug class.
Diltiazem is another non‑dihydropyridine calcium‑channel blocker with a milder negative‑inotropic effect, making it a better choice for patients with mild‑to‑moderate heart failure.
Amlodipine belongs to the dihydropyridine subclass. It strongly dilates peripheral vessels, so it’s preferred for isolated hypertension but offers little rate‑control benefit.
Metoprolol is a cardioselective beta‑blocker that reduces heart‑rate and myocardial oxygen demand, useful for angina and arrhythmias, but can worsen bronchospasm in asthmatics.
Atenolol is another beta‑blocker with a longer half‑life, often chosen for once‑daily dosing in hypertension.
Lisinopril is an ACE inhibitor that lowers blood pressure by blocking angiotensin‑II formation; it’s kidney‑protective but can cause cough and angioedema.
Nifedipine is a rapid‑acting dihydropyridine useful for hypertensive emergencies, though it may trigger reflex tachycardia.
Nitroprusside is an intravenous vasodilator reserved for acute crises; not a daily alternative but worth mentioning for completeness.
Side‑by‑Side Comparison
| Drug | Class | Main Indications | Typical Dose (adult) | Major Side Effects | Contra‑indications | Average Monthly Cost (US) |
|---|---|---|---|---|---|---|
| Verapamil (Isoptin) | Non‑dihydropyridine CCB | Hypertension, angina, SVT rate control | 80‑240mg PO qd or bid | Constipation, bradycardia, edema | Severe LV dysfunction, SA block | $12‑$20 |
| Diltiazem | Non‑dihydropyridine CCB | Angina, AF rate control, HTN | 120‑360mg PO qd | Headache, edema, AV block | 2nd/3rd degree AV block | $10‑$18 |
| Amlodipine | Dihydropyridine CCB | Isolated hypertension | 5‑10mg PO qd | Puffy ankles, flushing | Severe aortic stenosis | $8‑$15 |
| Metoprolol | Beta‑blocker | Hypertension, angina, post‑MI | 50‑200mg PO qd or bid | Fatigue, bradycardia, bronchospasm | Severe asthma, AV block | $5‑$12 |
| Lisinopril | ACE inhibitor | Hypertension, diabetic nephropathy | 10‑40mg PO qd | Cough, hyperkalemia, angioedema | Pregnancy (2nd/3rd trimester) | $4‑$9 |
| Nifedipine (ER) | Dihydropyridine CCB | Hypertension, angina | 30‑90mg PO qd | Headache, reflex tachycardia | Severe aortic stenosis | $7‑$14 |
How to Choose the Right Option
Pick a medication by weighing three practical factors:
- Clinical goal - Do you need blood‑pressure lowering, angina relief, or heart‑rate control? Verapamil shines when you need both BP+rate control.
- Patient comorbidities - Heart failure favors Diltiazem over Verapamil; asthma pushes you toward ACE inhibitors instead of beta‑blockers.
- Side‑effect tolerance & cost - Constipation is a deal‑breaker for many; cheap generics like Metoprolol may win for budget‑conscious patients.
Below are quick recommendations:
- For 55‑year‑old with hypertension+paroxysmal atrial fibrillation, preserved LV function: Verapamil or Diltiazem - choose based on constipation risk.
- For 68‑year‑old with hypertension+moderate heart failure (EF35%): Amlodipine or ACE inhibitor - avoid non‑dihydropyridine CCBs.
- For a young adult with isolated hypertension, wants once‑daily pill: Amlodipine or Lisinopril - beta‑blocker optional.
Switching from Verapamil - A Practical Checklist
- Confirm the new drug’s class and dosage equivalence with your prescriber.
- Gradually taper Verapamil over 3‑7days to avoid rebound hypertension.
- Schedule baseline vitals (BP, HR) and an ECG 24‑48hrs after the switch.
- Monitor for new side effects - e.g., cough with ACE inhibitors, edema with dihydropyridines.
- Re‑assess after 2weeks; adjust dose if BP>140/90mmHg or HR>80bpm.
Frequently Asked Questions
Can I take Verapamil and a beta‑blocker together?
Yes, but only under strict medical supervision. The combination can cause excessive bradycardia or AV block, so dose adjustments and frequent heart‑rate checks are essential.
Why does Verapamil cause constipation?
Verapamil slows smooth‑muscle activity throughout the GI tract, reducing peristalsis. Increasing dietary fiber, fluid intake, or adding a mild stool softener often helps.
Is Verapamil safe during pregnancy?
It is classified as Category C. Animal studies show risk, but human data are limited. Doctors typically avoid it unless the benefit clearly outweighs potential fetal harm.
What is the main difference between Verapamil and Diltiazem?
Both are non‑dihydropyridine CCBs, but Diltiazem has a milder negative‑inotropic effect, making it safer for patients with mild heart failure. Verapamil offers stronger AV‑node slowing, so it’s preferred for certain arrhythmias.
Which alternative is cheapest for long‑term hypertension?
Generic Metoprolol and Lisinopril typically cost under $10 per month, making them the most budget‑friendly choices compared with Verapamil’s $12‑$20 range.

Jonathan Mbulakey
October 3, 2025 AT 18:54Verapamil’s mechanism of action hinges on blocking L-type calcium channels in both cardiac and vascular smooth muscle.
By reducing intracellular calcium, the drug causes vasodilation, lowers peripheral resistance, and slows conduction through the AV node.
This tripartite effect makes it suitable for hypertension, angina, and certain supraventricular tachyarrhythmias.
However, the negative inotropic property can depress myocardial contractility, an important caveat in patients with reduced ejection fraction.
Clinical guidelines therefore reserve verapamil for cases where beta‑blockers are contraindicated or ineffective.
The drug’s half‑life of around three to seven hours permits once‑ or twice‑daily dosing, depending on the formulation.
Generic versions are priced between twelve and twenty dollars per month, which is modest but higher than many first‑line agents.
Side‑effect profile includes constipation, dizziness, and a noteworthy risk of bradycardia, especially when combined with other rate‑controlling agents.
The constipation stems from reduced smooth‑muscle motility throughout the gastrointestinal tract, a phenomenon readily mitigated by dietary fiber or stool softeners.
In terms of drug interactions, verapamil is a potent CYP3A4 inhibitor, raising plasma levels of statins, certain anti‑arrhythmics, and some antihistamines.
Physicians must therefore monitor for signs of toxicity when prescribing concomitant medications that share this metabolic pathway.
When comparing alternatives, diltazem offers a milder negative‑inotropic effect while preserving similar efficacy in rate control.
Amlodipine, a dihydropyridine calcium channel blocker, excels at blood‑pressure reduction but lacks significant AV‑node slowing, making it less ideal for arrhythmia management.
Beta‑blockers such as metoprolol provide robust heart‑rate control and are generally cheaper, yet they may exacerbate bronchospasm in asthmatic patients.
ACE inhibitors like lisinopril are first‑line for hypertension and possess renal protective properties, though they can provoke a dry cough.
Ultimately, the choice among these agents hinges on the patient’s comorbidities, cost considerations, and tolerance of side effects, underscoring the importance of individualized therapy.
Roxanne Porter
October 4, 2025 AT 03:14The comparison chart rightly highlights that verapamil excels in AV‑node suppression relative to many alternatives.
Yet the higher incidence of heart‑failure exacerbation cannot be ignored, especially in older cohorts.
Diltazem’s gentler impact on contractility often makes it the preferred non‑dihydropyridine when cardiac output is marginal.
For pure blood‑pressure control without arrhythmic concerns, amlodipine remains cost‑effective and well‑tolerated.
It is prudent for clinicians to align drug selection with the dominant clinical indication rather than defaulting to a single agent.
Abby VanSickle
October 4, 2025 AT 11:34Verapamil’s cost is higher than most generic antihypertensives, which may affect adherence.
Carys Jones
October 4, 2025 AT 19:54Banning verapamil outright because of a handful of side‑effects would be an outright medical overreach.
Nonetheless, glorifying it as a miracle cure while ignoring its heart‑failure risks reads like a promotional pamphlet.
Patients deserve balanced information that does not tip the scales toward hype.
The article’s neutral tone helps, but some of the bullet points downplay the seriousness of bradycardia.
Warren Neufeld
October 5, 2025 AT 04:14The points made are clear and straightforward.
Verapamil can help some patients but needs careful monitoring.
Doctors should weigh benefits against risks each time.
Keisha Moss Buynitzky
October 5, 2025 AT 12:34The pharmacodynamic profile of verapamil underscores its utility in specific cardiac indications.
Its contraindication in severe left‑ventricular dysfunction aligns with current consensus statements.
Moreover, the drug’s interaction potential via CYP3A4 necessitates vigilant prescribing practices.
In sum, verapamil remains a valuable option when deployed judiciously.
Shivam yadav
October 5, 2025 AT 20:54In many South Asian practices, calcium‑channel blockers are often the first line for hypertension due to dietary sodium patterns.
Verapamil, however, is prescribed cautiously because the prevalence of heart‑failure in the region is rising.
Patients frequently report constipation, prompting clinicians to advise increased fiber intake.
Combining verapamil with a low‑dose beta‑blocker can be effective if the heart rate is closely observed.
Ultimately, education on medication adherence is as important as the drug choice itself.
pallabi banerjee
October 6, 2025 AT 05:14Your cultural insights add valuable context to the discussion.
It is true that dietary habits influence treatment strategies.
Monitoring for side effects remains essential regardless of geography.
Collaborative care models help tailor therapy to individual needs.
Alex EL Shaar
October 6, 2025 AT 13:34Yo, this verapamil thing is a real mixed bag, ain’t it?
You got the hype for heart‑rate control, but then the heart‑failure risk slaps you right in the face.
And don’t even get me started on that cursed constipation that makes you feel like a turtle on a treadmill.
If you’re looking for cheap meds, you might as well grab a generic metoprolol and save a buck.
The drug‑drug interaction list reads like a novel, especially with statins lurking in the background.
Bottom line: use it only if you’ve got a solid monitoring plan, otherwise you’re just signing up for trouble.
Anna Frerker
October 6, 2025 AT 21:54Short and sweet, I agree.
Monitoring is key.
Kim Nguyệt Lệ
October 7, 2025 AT 06:14The article correctly distinguishes between calcium‑channel blocker subclasses.
However, the bullet points could benefit from parallel structure.
For instance, “High Blood Pressure Control” should be consistent across all entries.
Additionally, the phrase “severe left‑ventricular dysfunction (ejection fraction 140/90mmHg or HR>80bpm.” contains a typographical error.
Rhonda Adams
October 7, 2025 AT 14:34Great job summarizing the key differences, everyone! 😊
Remember, switching meds should always be done with a taper plan to avoid rebound hypertension.
It helps to keep a medication diary noting blood pressure trends and any side effects.
Stay informed and keep the conversation going-your health journey matters! 👍
Macy-Lynn Lytsman Piernbaum
October 7, 2025 AT 22:54Wow, that’s a lot of info in one post! 🤯
Verapamil’s AV‑node slowdown is super useful for atrial fibrillation, but the constipation can be a pain.
If cost is a concern, metoprolol or lisinopril might be the way to go.
Always chat with your doc before making any changes, okay? 🙌
Alexandre Baril
October 8, 2025 AT 07:14Thanks for the clear breakdown of each medication.
It’s helpful to see side‑effects listed side‑by‑side.
This will make my next appointment with the cardiologist much easier.
Stephen Davis
October 8, 2025 AT 15:34Picture this: a heart that’s a smooth jazz band, verapamil is the mellow sax that keeps the tempo steady.
Diltazem, on the other hand, is the laid‑back bassist, less likely to pull the rug out from under the rhythm.
If you’re after a budget‑friendly tune, metoprolol drops the beat without breaking the bank.
Meanwhile, amlodipine bursts onto the stage with vasodilatory fireworks, dazzling the crowd.
Choose your instrument wisely, because every orchestra needs the right harmony.
Grant Wesgate
October 8, 2025 AT 23:54The comparison tool is user‑friendly and visually appealing.
It succinctly presents effectiveness and side‑effect data.
I appreciate the inclusion of price ranges for each drug.
Keep up the good work! 🎉
Richard Phelan
October 9, 2025 AT 08:14Behold, the saga of verapamil versus its comrades, a battle of calcium channels!
In the left‑hand corner, verapamil wields its AV‑node crushing might, while the right‑hand contender, diltazem, dances with a gentler touch.
The crowd gasps as amlodipine flares up with vasodilatory fireworks, stealing the spotlight for pure hypertension.
Metoprolol enters the arena, a stoic warrior, cheap and reliable, yet threatened by the dreaded cough of ACE inhibitors looming nearby.
Let the clinician be the wise arbiter, lest the drama devolve into patient peril.
benjamin malizu
October 9, 2025 AT 16:34From a pharmacokinetic perspective, verapamil exhibits a moderate elimination half‑life, necessitating BID dosing in certain formulations.
Its CYP3A4 inhibition profile precipitates clinically significant drug‑drug interactions, especially with statin metabolism.
Hemodynamically, the negative inotropic effect mandates vigilant ejection fraction monitoring in systolic dysfunction cohorts.
Comparative efficacy analyses reveal non‑inferiority to diltazem in rate control metrics, albeit with a heightened adverse event signal.
Thus, therapeutic decision‑making should integrate pharmacoeconomic assessments alongside patient‑centred outcome measures.
Maureen Hoffmann
October 10, 2025 AT 00:54Wow, what a comprehensive rundown-kudos to the author for pulling all this together!
If you’re wrestling with constipation on verapamil, try adding a high‑fiber snack and plenty of water.
For those whose hearts can’t handle the negative inotropy, diltazem or an ACE inhibitor might be a safer harbor.
Remember, the cheapest option isn’t always the best if side‑effects send you back to the doctor.
Keep sharing your experiences; community wisdom is a powerful ally on the road to better health!