Ever taken a pill and wondered if it really worked because you ate right after? Or maybe you skipped a meal to take your medicine, only to feel sick afterward? You’re not alone. Many people don’t realize that what you eat - and when you eat it - can make your medication work better, worse, or even cause side effects. The truth is, food-drug interactions aren’t just a footnote in the pill bottle. They can change how much of your medicine gets into your bloodstream, how fast it kicks in, and whether it’s safe at all.
Why Food Changes How Medicines Work
Your digestive system doesn’t just break down your breakfast. It also decides how much of your medicine actually makes it into your blood. When food enters your stomach, it triggers a chain reaction: your stomach empties slower, your gut pH shifts, bile production increases, and blood flow to your intestines changes. All of this affects how your body absorbs drugs. For example, high-fat meals can delay gastric emptying by up to two hours. That means a painkiller like acetaminophen might take twice as long to reach its peak level in your blood if you take it after a greasy burger. On the flip side, some drugs need fat to be absorbed at all. Griseofulvin, an antifungal used for nail infections, absorbs 200-300% better with a high-fat meal because bile - released in response to fat - helps dissolve the drug so your body can use it. Other interactions are more dangerous. Tetracycline antibiotics, often prescribed for acne or infections, bind to calcium in dairy products like milk, yogurt, or cheese. This creates an insoluble compound your body can’t absorb. Studies show this cuts the drug’s effectiveness by 50-75%. One Reddit user shared how their recurring UTI didn’t clear up until they stopped taking doxycycline with their morning yogurt. Two hours apart made all the difference.Empty Stomach vs. With Food: What’s the Real Difference?
Doctors and pharmacists often tell you to take your medicine on an empty stomach or with food. But what does that actually mean? Empty stomach means no food for at least one hour before and two hours after taking the pill. This isn’t just a suggestion - it’s a requirement for certain drugs. Levothyroxine, used to treat hypothyroidism, is a prime example. Food can reduce its absorption by 30-55%. That means even if you take your dose at the same time every day, eating breakfast too soon after can leave you with low thyroid hormone levels, causing fatigue, weight gain, and brain fog. Mount Elizabeth Hospital’s guidelines say you should take it with plain water only, at least 30 minutes before your first bite of food. With food doesn’t always mean a full meal. For some drugs, even a small snack of 200-300 calories is enough. Nitrofurantoin, a urinary tract infection treatment, absorbs 40% better when taken with food. Same with cefpodoxime - its absorption jumps by 50-60% when paired with a meal. And for NSAIDs like ibuprofen, taking them with food cuts stomach irritation from 42% of users down to just 12%, according to a GoodRx survey of 5,000 people. But here’s the catch: some medications need food to be absorbed, but too much fat can hurt. Itraconazole, another antifungal, requires an acidic environment in the stomach to work. High-fat meals raise stomach pH, making it less acidic. That drops absorption by 40%. So even if you’re told to take it with food, a heavy meal could make it useless.Timing Matters More Than You Think
It’s not just about whether you eat - it’s when. For some drugs, the exact minute you take them relative to your meal makes or breaks the treatment. Take glipizide, a sulfonylurea used for type 2 diabetes. This drug tells your pancreas to release insulin. If you take it on an empty stomach, your blood sugar can crash - below 70 mg/dL - within hours. The American Diabetes Association found that 23% of patients who took this medication without eating had symptoms severe enough to need medical help. The fix? Take it 30 minutes before your meal. That way, insulin rises just as your blood sugar starts climbing from food. Semaglutide (Ozempic, Wegovy) is another timing-sensitive drug. Novo Nordisk’s clinical trials showed that taking it within 30 minutes of your first bite reduces absorption by 44%. That’s a huge drop in effectiveness. The label says to take it at least 30 minutes before eating. Set a phone alarm. Mark it on your calendar. This isn’t optional. Even medications that seem harmless - like certain HIV drugs or cholesterol pills - can be affected. Some antiretrovirals need a light snack to reduce nausea, but a heavy meal can spike their levels too high, increasing side effects. The FDA now requires food-effect data for 35% of all new drugs approved since 2015. That’s not a small number. It means nearly one in three prescriptions you get today has specific food rules built into its design.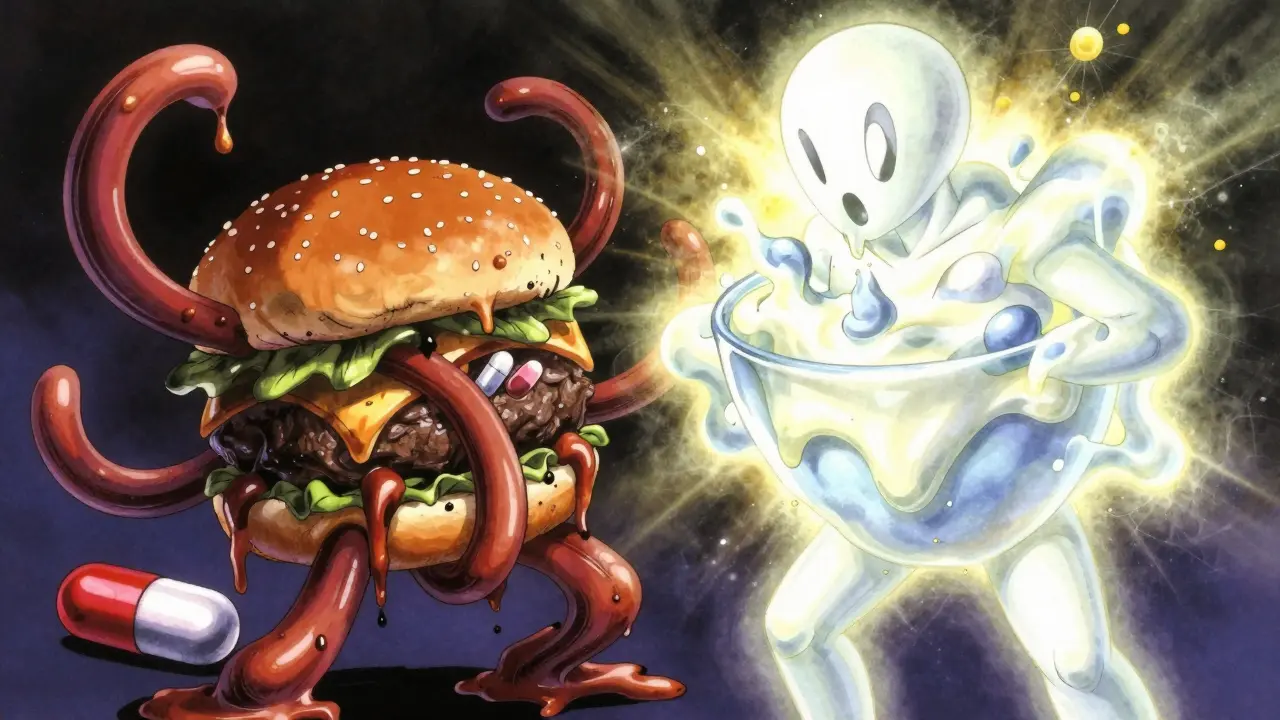
What the Experts Say - And Why They Disagree
Not all guidelines line up perfectly. That’s where confusion creeps in. The Australian Prescriber (2023) says for most chronic medications - like blood pressure pills or antidepressants - the exact timing relative to meals doesn’t matter as long as you’re consistent. If you always take your lisinopril with dinner, that’s fine. Your body adapts. The goal is steady levels over time, not perfect absorption every single dose. But for others - like levothyroxine, antibiotics, or diabetes drugs - consistency isn’t enough. Absorption must be optimal. That’s why Mount Elizabeth Hospital and the Mayo Clinic stress that for these drugs, empty stomach isn’t a preference - it’s a medical necessity. Even NSAIDs are a gray area. Some sources say take them with food to protect your stomach. Others say if it’s enteric-coated (a special coating that dissolves in the intestine, not the stomach), you can skip the food. MyDr.com.au recommends food to prevent acid reflux. The American College of Gastroenterology says it’s optional. The difference? The type of pill you’re holding. Bottom line: don’t assume. Check your label. Ask your pharmacist. If the instructions say “with food,” ask: how much? What kind? When?Real People, Real Mistakes
Behind every guideline is a person trying to follow it. On Drugs.com, 62% of users taking levothyroxine admitted they struggled to take it on an empty stomach. Many just grabbed a coffee and a bagel right after their pill. Result? Persistent fatigue, weight gain, and depression - symptoms they thought were “just aging.” Once they fixed their timing, their thyroid levels normalized. Express Scripts’ 2023 report found that 45% of patients misunderstand “take with food.” They think it means a full meal. For drugs like certain antiretrovirals, a banana or a handful of crackers is enough. A full breakfast might make the drug less effective or cause nausea. And then there’s the elderly. People over 65 are more likely to take five or more medications daily. A 2022 study in the Journal of the American Geriatrics Society found they have a 65% higher risk of food-drug interactions. Mix a calcium supplement with an antibiotic. Take a blood pressure pill with grapefruit juice. Skip breakfast before a diabetes drug. These aren’t just mistakes - they’re dangerous.
How to Get It Right - Practical Tips
Here’s how to avoid the most common errors:- Use a pill organizer with time slots. Separate “before meals,” “with meals,” and “after meals.”
- Set phone alarms. One alarm 60 minutes before breakfast for levothyroxine. Another 30 minutes before lunch for glipizide.
- Ask your pharmacist to write it down. Don’t rely on memory. Get the instructions in plain language: “Take with a small snack,” “Wait 2 hours after dairy,” “Take 1 hour before food.”
- Check for food warnings on your prescription label. Look for phrases like “avoid grapefruit,” “do not take with milk,” or “take with food.”
- Don’t assume all pills are the same. One brand of ibuprofen may be enteric-coated. Another isn’t. Always check the specific drug name and formulation.
- Use apps like Medisafe or MyTherapy. They send reminders for food timing and track adherence. Users who turned on food reminders saw 27% fewer timing errors.
What’s Changing in 2025
The rules are evolving. The FDA now requires food-effect testing using plant-based and gluten-free meals - not just greasy burgers - to reflect modern diets. In 2023, a Lancet Digital Health study showed that timing levothyroxine based on individual gastric emptying rates (measured with a simple breath test) improved outcomes by 22% compared to the standard one-hour rule. Digital tools are catching up, too. Companies like Medtronic are testing ingestible sensors that track stomach pH and emptying in real time. Imagine your phone pinging: “Your stomach is ready. Take your pill now.” That’s not science fiction anymore. And in January 2024, the American Society of Health-System Pharmacists updated guidelines to replace vague terms like “with food” with precise language: “within 30 minutes of starting your meal” or “minimum 60 minutes before first bite.” This standardization will help reduce confusion across hospitals and pharmacies.Final Takeaway: Food Isn’t Just Fuel - It’s Part of Your Treatment
Your medication doesn’t work in a vacuum. It works in your body - and your body is shaped by what you eat, when you eat it, and how your digestion responds. Getting the timing right isn’t about being perfect. It’s about being consistent, informed, and intentional. If you’re on more than one medication - especially for chronic conditions - ask your pharmacist: “Does food affect any of these?” Write it down. Set reminders. Track your symptoms. That small step can mean the difference between feeling better… and wondering why you’re still sick.The science is clear: food and medicine are partners. Sometimes they help each other. Sometimes they fight. Know which is which.

