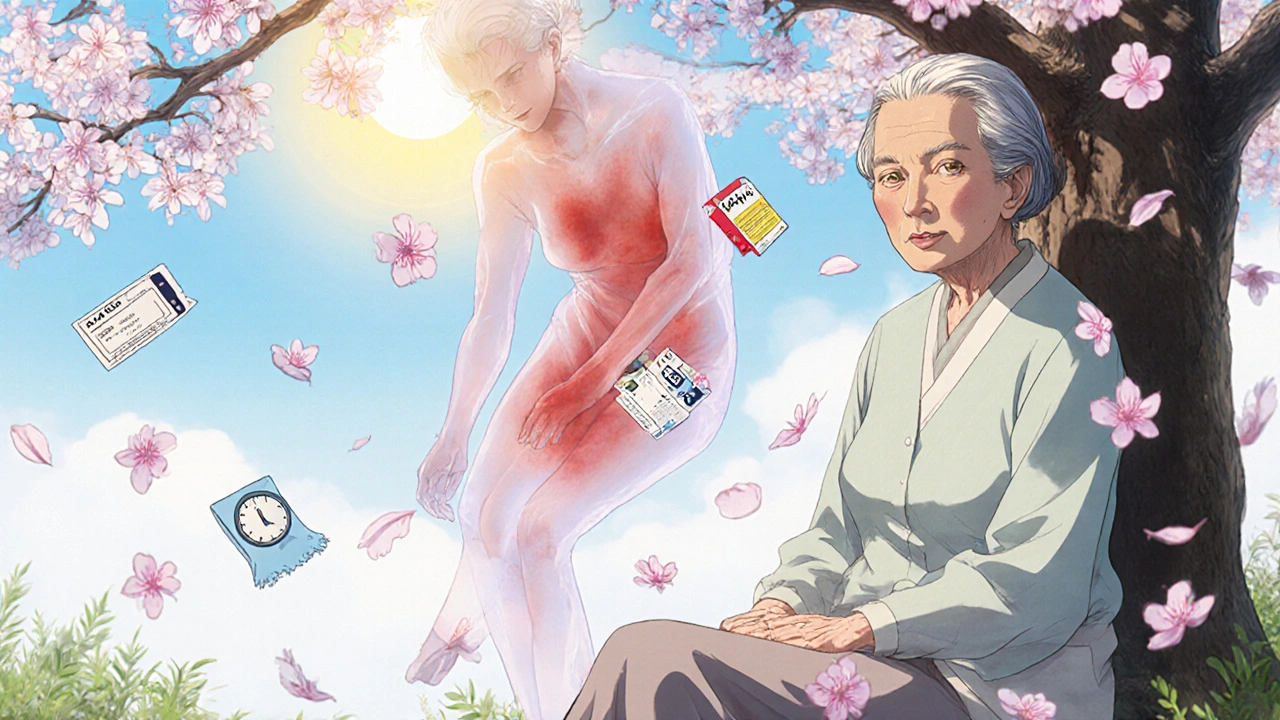
More than 1,000 common medications can make your skin dangerously sensitive to the sun-even on cloudy days or through windows. If you're taking antibiotics, blood pressure pills, or even over-the-counter pain relievers, you might be at risk for a reaction you didn’t know existed. This isn’t just a bad sunburn. It’s medication photosensitivity, and it can lead to blisters, long-lasting dark spots, or even raise your risk of skin cancer.
What Exactly Is Medication Photosensitivity?
Medication photosensitivity happens when a drug in your body reacts with sunlight, especially UVA rays (320-400 nm). These rays penetrate deeper than UVB, which is what causes typical sunburns. The reaction isn’t an allergy in the usual sense-it’s a chemical one. Think of it like your skin turning into a solar panel for the drug, absorbing light and turning it into damaging energy. There are two main types:- Phototoxic reactions (95% of cases): These happen fast-within minutes to a few hours after sun exposure. Your skin looks like a bad sunburn: red, swollen, painful, sometimes blistering. It only shows up where the sun hit you.
- Photoallergic reactions (5% of cases): These are slower and trickier. They show up 1-3 days after exposure, often spreading beyond sun-exposed areas. The rash looks like eczema-itchy, flaky, and can show up on your neck, chest, or even under clothes.
One key difference? Phototoxicity can happen to anyone who takes enough of the drug and gets enough sun. Photoallergy only affects people whose immune systems have been sensitized to the drug first-so it’s rarer, but harder to predict.
Which Medications Cause the Most Problems?
You might be surprised how many everyday drugs carry this risk. Here are the top offenders:- Tetracyclines (like doxycycline): Used for acne, Lyme disease, and infections. Up to 20% of users get phototoxic burns-even through light clothing.
- NSAIDs (like ketoprofen, ibuprofen): Especially topical gels. A single application can trigger a reaction if you go outside.
- Fluoroquinolones (like ciprofloxacin): Common antibiotics for UTIs and sinus infections. Reactions can be severe.
- Amiodarone (Cordarone): A heart medication. Up to 75% of long-term users develop lasting skin discoloration that can stick around for decades.
- Sulfonamides and phenothiazines: Used for infections and mental health conditions. These are the most common triggers for photoallergy.
Even some sunscreen ingredients-like oxybenzone-can cause photoallergic reactions. Yes, the product meant to protect you can sometimes make things worse.
Why Most People Don’t Know They’re at Risk
You won’t find a warning on the pill bottle unless it’s one of the 200+ high-risk drugs the FDA now requires to carry a photosensitivity alert. But here’s the problem: 68% of patients get no sun safety advice when they’re prescribed these medications.One Reddit user, a pharmacist named 'SunburnedPharmD,' described getting severe burns during a 15-minute walk after starting doxycycline. No doctor warned her. She thought it was just a bad sunburn-until her skin blistered.
Studies show most people apply less than half the recommended amount of sunscreen. If you’re on a photosensitizing drug, that’s not enough. You need more than SPF 30. You need SPF 50+, zinc oxide, and a whole new approach to sun exposure.

How to Protect Yourself-For Real
Forget the old advice. If you’re on a medication that causes photosensitivity, you need to treat sun exposure like a medical risk. Here’s what actually works:- Use zinc oxide or titanium dioxide sunscreens-SPF 50+ minimum. Look for "broad-spectrum" and check the ingredients. Avoid chemical filters like avobenzone alone-they don’t block UVA well enough.
- Apply 1 ounce (a shot glass full) for your whole body. Most people use ¼ of that. Reapply every 2 hours, or after sweating or wiping your skin.
- Wear UPF 50+ clothing. A regular white T-shirt blocks only 3-5% of UV. UPF 50+ clothing blocks 98%. Brands like Solbari and Coolibar are tested and trusted. Long sleeves, wide-brimmed hats, and UV-blocking sunglasses are non-negotiable.
- Check the UV index daily. Use apps like UVLens. If it’s 3 or higher, plan your outdoor time before 10 a.m. or after 4 p.m. Even a 15-minute walk can be dangerous if you’re on doxycycline.
- Stay in the shade. UVA rays go through clouds, windows, and light fabrics. Sitting under an umbrella? Still at risk. You need physical barriers.
Patients who followed this full protocol saw a 57% drop in severe reactions, according to the Cleveland Clinic. Those who just used regular sunscreen? Not much change.
What to Do If You React
If your skin turns red, burns, or blisters after sun exposure:- Get out of the sun immediately.
- Cool the area with damp cloths-no ice.
- Use a fragrance-free moisturizer or hydrocortisone cream (1%) for itching.
- Don’t pop blisters. They protect the skin underneath.
- Call your doctor. Tell them exactly what meds you’re on and when the reaction started.
For photoallergic reactions, you may need a short course of oral steroids. For phototoxic burns, healing can take weeks. And in some cases-like with amiodarone-the dark spots never fully fade.
What’s Changing in 2025
The field is evolving fast:- The FDA now requires photosensitivity warnings on over 200 medications.
- Companies like 23andMe offer genetic tests that can tell you if you’re more likely to react (based on MC1R gene variants).
- "Smart" sunscreens that change color when UV exposure gets dangerous are in prototype testing.
- Photoprotectin, a new oral drug that reduces UV-induced skin damage by 70%, was approved in 2023.
But here’s the catch: most primary care doctors still don’t screen for this. Only 35% do. Dermatologists? 85%. If you’re on a long-term medication, ask your doctor: "Could this make me more sensitive to the sun?" Don’t wait for a reaction.
Real People, Real Results
One user on MyHealthTeams, "UVWarrior," switched to UPF 50+ clothing after three severe phototoxic reactions. "I went from needing emergency care every summer to hiking without fear," they said. "It’s not about avoiding the sun-it’s about protecting yourself right."Another, a 72-year-old on amiodarone, started using zinc oxide sunscreen and wearing a wide-brimmed hat every day. "My skin hasn’t darkened in 18 months," she told her dermatologist. "I didn’t know I could stop it."
Final Thought: This Isn’t Just About Sunburn
Medication photosensitivity isn’t a minor side effect. It’s a hidden risk that affects millions. The Skin Cancer Foundation says it can increase your risk of non-melanoma skin cancer by up to 60%. That’s not a small number.By 2030, climate change will make UV levels even higher. More people will be on more medications. Without better awareness, this problem will grow.
Know your meds. Know your skin. Protect yourself like your life depends on it-because for some, it does.
Can I still go outside if I’m on a photosensitizing medication?
Yes, but you need to be smarter about it. Avoid direct sun between 10 a.m. and 4 p.m. when UV is strongest. Wear UPF 50+ clothing, a wide-brimmed hat, and broad-spectrum SPF 50+ sunscreen with zinc oxide. Check the UV index daily. You don’t have to stay indoors-just protect yourself like you’re handling a chemical hazard.
Is regular sunscreen enough?
No. Most SPF 30 sunscreens don’t block enough UVA rays-the kind that cause phototoxic reactions. You need SPF 50+ with zinc oxide or titanium dioxide as the main active ingredients. Also, most people apply too little. Use a full ounce (shot glass) for your body and reapply every 2 hours. If you’re on a high-risk drug, don’t rely on sunscreen alone-combine it with clothing and shade.
How long does photosensitivity last after stopping the medication?
It depends on the drug. For most, the risk fades within days or weeks after stopping. But for drugs like amiodarone, photosensitivity can last for years-even decades. The drug stores in fat tissue and slowly releases. If you’ve taken it long-term, assume you’re still at risk and keep protecting your skin.
Can I use tanning beds if I’m on these medications?
Absolutely not. Tanning beds emit intense UVA radiation-often stronger than the midday sun. If you’re on a photosensitizing drug, tanning beds can cause severe burns, blistering, and long-term skin damage in minutes. There’s no safe level of artificial UV exposure if you’re on these medications.
Should I get a skin check if I’ve had a reaction?
Yes. Repeated phototoxic or photoallergic reactions increase your risk of non-melanoma skin cancers like basal cell carcinoma and squamous cell carcinoma. See a dermatologist for a full skin exam, especially if you’ve had multiple reactions or are on long-term medications like amiodarone. Early detection saves lives.
Are natural or mineral sunscreens better for photosensitivity?
Yes. Mineral sunscreens with zinc oxide or titanium dioxide sit on top of the skin and physically block UVA and UVB rays. Chemical sunscreens absorb UV and can break down faster, sometimes even triggering photoallergic reactions themselves. For photosensitivity, mineral is the gold standard. Look for at least 15% zinc oxide.
Can I use makeup or lotions while on these meds?
Be careful. Some makeup, perfumes, and lotions contain photosensitizing ingredients like citrus oils, lavender, or musk. Avoid products with fragrances if you’re on high-risk meds. Stick to fragrance-free, hypoallergenic formulas. Always patch-test new products on a small area before full use.
Is there a test to confirm I have medication-induced photosensitivity?
Yes, it’s called photopatch testing. A dermatologist applies small amounts of common photosensitizers to your skin and exposes them to controlled UV light. But this test only confirms the cause in 30-40% of cases. The most reliable tool is your medication history. If a reaction happened after starting a new drug and cleared after stopping it, that’s strong evidence. Don’t wait for a test-talk to your doctor.


Pawan Jamwal
November 19, 2025 AT 18:22Bill Camp
November 20, 2025 AT 05:37Matthew McCraney
November 22, 2025 AT 04:41serge jane
November 24, 2025 AT 01:47Nick Naylor
November 24, 2025 AT 20:35Brianna Groleau
November 25, 2025 AT 16:39Rusty Thomas
November 26, 2025 AT 10:37Sarah Swiatek
November 26, 2025 AT 11:44Dave Wooldridge
November 28, 2025 AT 07:57Rebecca Cosenza
November 29, 2025 AT 21:18swatantra kumar
November 30, 2025 AT 11:35