Orthostatic Hypotension Medication Risk Calculator
Your Risk Factors
About Orthostatic Hypotension
Orthostatic hypotension occurs when your blood pressure drops by 20 mm Hg systolic or 10 mm Hg diastolic when standing up. This can cause dizziness, lightheadedness, or fainting.
- Age 70+ (3x higher risk)
- 4+ medications (5.7x higher risk)
- Diabetes or Parkinson's
- Dehydration
Standing up too fast and feeling like the room is spinning? That dizzy spell isn’t just bad luck-it could be your medications. Orthostatic hypotension, or low blood pressure when standing, is one of the most common and dangerous side effects of drugs taken by older adults. It’s not rare. It’s not minor. It’s the reason thousands of people fall each year, end up in the ER, or even suffer brain injuries from a simple trip to the bathroom.
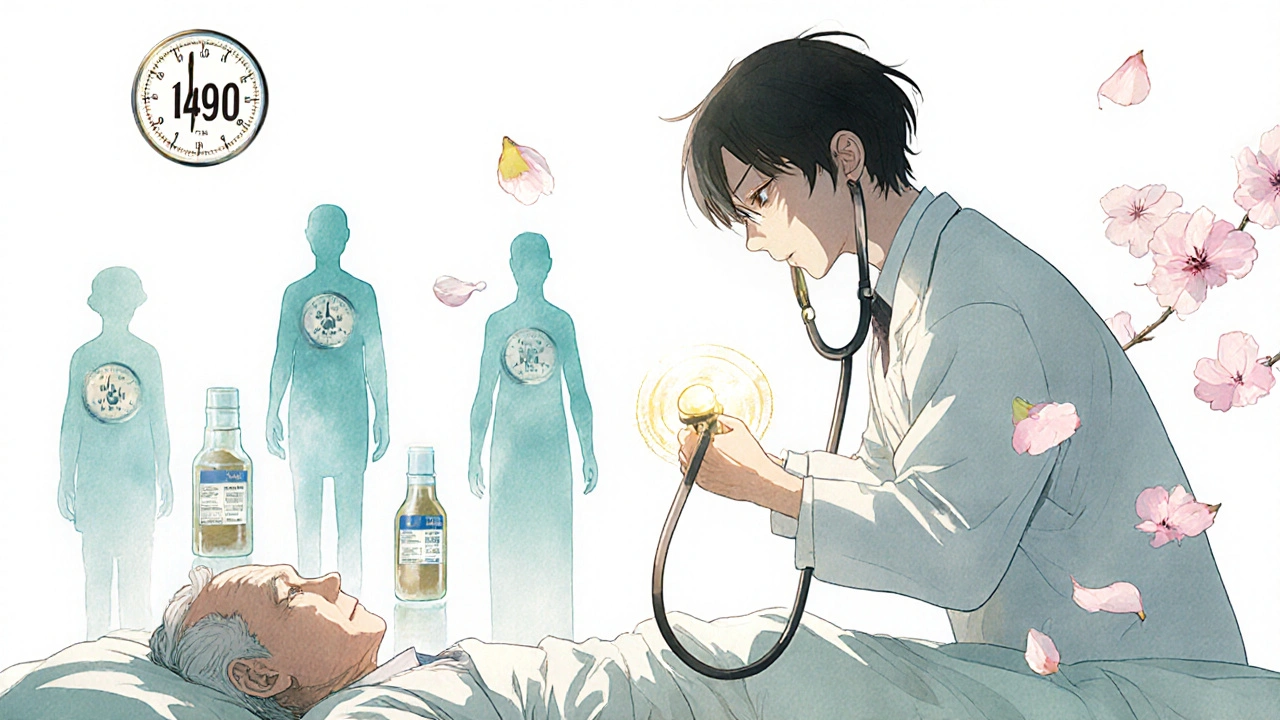
What Exactly Is Orthostatic Hypotension?
Orthostatic hypotension happens when your blood pressure drops too much within three minutes of standing up. The official medical definition? A drop of 20 mm Hg in systolic pressure (the top number) or 10 mm Hg in diastolic pressure (the bottom number). That’s not a little lightheadedness-it’s your brain not getting enough blood. And when that happens, you feel dizzy, blurry, or like you’re about to pass out.It’s not just about being unsteady. Studies show people with this condition have a 15-30% higher risk of falling and a 24-32% increased chance of dying within 10 years. The worst part? Many don’t realize their meds are the cause. Symptoms often show up weeks or months after starting a new drug. By then, the damage-falls, fractures, hospital stays-has already happened.
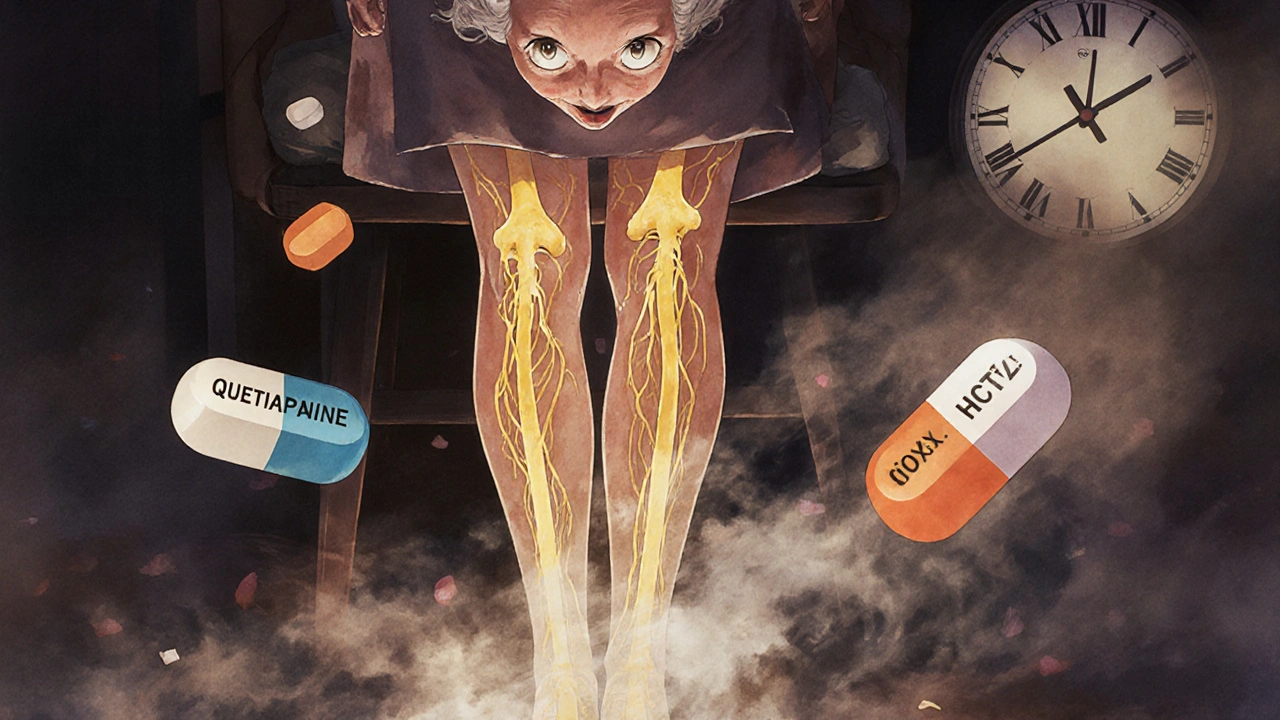
Which Medications Cause This?
Not all drugs cause this. But some do-and often without warning. Here are the biggest culprits, backed by clinical data:- Antipsychotics like clozapine, quetiapine, and chlorpromazine: Up to 40% of older patients on these develop orthostatic hypotension. Quetiapine, commonly prescribed for anxiety or sleep, is especially risky. One Reddit user reported fainting twice after starting it, with blood pressure dropping from 128/82 to 92/61 in under two minutes.
- Opioids like oxycodone and morphine: These cause dizziness in 15-25% of elderly users. The risk doubles if combined with alcohol or benzodiazepines.
- Diuretics like hydrochlorothiazide: These drain fluid from your body, reducing blood volume. One patient’s recurrent falls stopped completely after stopping HCTZ-within 72 hours.
- Alpha-blockers like doxazosin and terazosin: Used for high blood pressure or prostate issues, these relax blood vessels too much. They’re linked to a 2.8 times higher risk of OH.
- Tricyclic antidepressants like amitriptyline: These interfere with nerve signals that control blood pressure. Risk jumps 3.2 times compared to other antidepressants.
- Levodopa for Parkinson’s: Up to half of patients on this drug develop OH. It’s so common, doctors expect it.
It’s not about one drug alone. The real danger comes from stacking them. People over 70 who take four or more medications have a 5.7 times higher risk than those on one or two. Polypharmacy isn’t just a buzzword-it’s a ticking time bomb.
Why Does This Happen?
Your body normally adjusts when you stand. Blood vessels tighten, heart rate increases, and your brain stays fed. But medications mess with this system. Some block the nerves that tell your blood vessels to squeeze. Others drain fluid. Some slow down your brain’s response to low pressure. The result? Blood pools in your legs. Your brain gets starved. You feel dizzy.It’s not your fault. Your body isn’t failing-it’s being overpowered by drugs meant to help. The irony? Many of these medications treat serious conditions: high blood pressure, depression, chronic pain, Parkinson’s. But if they make you fall, are they really helping?
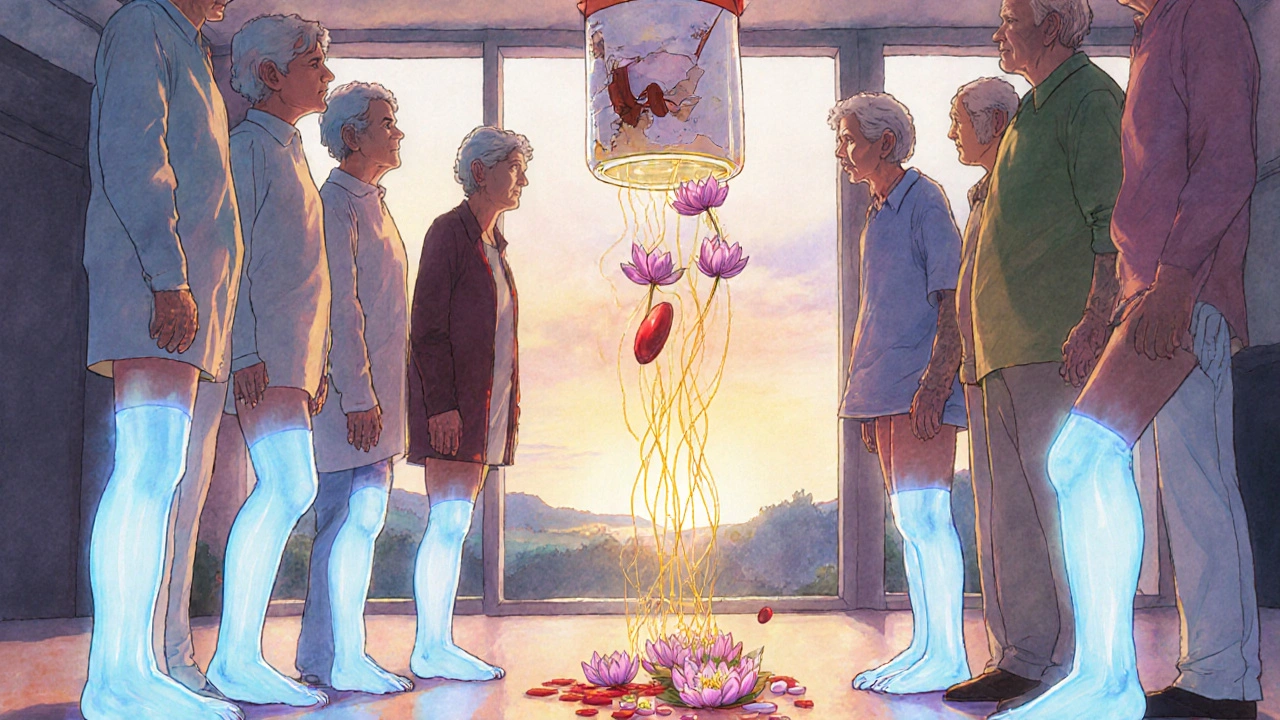
Who’s Most at Risk?
You’re not equally vulnerable. Risk climbs with age, other health problems, and how many pills you take:- Age 70+: Three times more likely than younger adults.
- Four or more medications: Over five times higher risk.
- Diabetes or Parkinson’s: These damage the nerves that control blood pressure.
- Dehydration: Even mild fluid loss makes OH worse.
- Alcohol use: It amplifies the effect of many OH-causing drugs.
Many patients don’t realize they’re at risk until they’ve already fallen. That’s why routine screening matters. The American Geriatrics Society now lists 12 high-risk drugs in its Beers Criteria-guidelines used by 68% of U.S. primary care clinics.
How Is It Diagnosed?
Doctors don’t guess. They measure. The standard test is simple:- Rest lying down for five minutes.
- Measure blood pressure and heart rate.
- Stand up.
- Measure again at 1, 2, and 3 minutes.
If your systolic pressure drops 20 mm Hg or more-or diastolic drops 10 mm Hg or more-and you feel dizzy at the same time, it’s orthostatic hypotension. But here’s the catch: up to 40% of people with this condition have no symptoms. They feel fine. But their blood pressure still crashes. That’s why doctors should check for it in anyone over 65 on multiple meds-even if they say they’re fine.
Many patients report symptoms lasting months before anyone connects the dots. One Mayo Clinic study found 55% of patients had dizziness for over two months before their meds were reviewed.
What Can You Do About It?
The good news? Medication-induced orthostatic hypotension is often reversible. About 70-85% of cases improve when the right drugs are adjusted.Here’s what works:
- Review your meds: Ask your doctor: “Could any of these be making me dizzy?” Don’t assume they know. Bring a list of everything you take-even supplements.
- Slow down: When standing, pause for 10-15 seconds after sitting up. Don’t jump out of bed. Sit on the edge first. Let your body catch up.
- Drink more water: Aim for 2-2.5 liters a day. Dehydration makes OH worse. Coffee and tea don’t count-they’re diuretics.
- Wear compression stockings: These help push blood back up from your legs. Studies show they reduce dizziness in over half of patients.
- Avoid heat: Hot showers, saunas, and hot days all dilate blood vessels and make OH worse.
- Don’t skip meals: Large meals can drop blood pressure. Eat smaller, more frequent meals.
For some, changing the drug helps. For example, switching from quetiapine to ziprasidone can cut OH risk from 35-45% down to 5-10%. Switching from doxazosin to a different blood pressure pill may remove the problem entirely.
When Medication Changes Aren’t Enough
If lifestyle changes don’t help, doctors may turn to medication. The American Heart Association now recommends midodrine as a first-line treatment. It’s a drug that tightens blood vessels. In trials, it reduced dizziness by 65%. But it’s not for everyone-it can cause high blood pressure when lying down. That’s why it’s only used after other options fail.There’s also new research coming. Seven pharmaceutical companies are developing next-gen drugs designed to treat conditions like high blood pressure or Parkinson’s without triggering OH. One approach targets specific receptors (alpha-1A) that control blood pressure without affecting others. These are still in trials-but they’re coming.
What Happens If You Ignore It?
Ignoring dizziness on standing isn’t just inconvenient. It’s dangerous. Falls are the leading cause of injury-related death in people over 65. A single fall can mean a hip fracture, hospitalization, loss of independence, or even death.Medicare spends $31 billion a year on fall-related care. About 30-40% of those costs come from drug-induced orthostatic hypotension. That’s not just a medical problem-it’s a financial one. And it’s preventable.
Every year, 1.5 million older adults are hospitalized because of falls linked to medication side effects. Most of these could be avoided with a simple medication review.
Final Thoughts: Don’t Accept Dizziness as Normal
Feeling dizzy when you stand up isn’t just part of getting older. It’s a warning sign. A red flag. A signal that your body is struggling under the weight of too many drugs.If you or someone you love is on multiple medications and feels lightheaded when standing, don’t wait. Don’t assume it’s harmless. Ask your doctor: “Could this be from my meds?” Bring your pill bottle. Ask about alternatives. Ask about non-drug options.
Medications save lives. But they can also put them at risk. The goal isn’t to stop all treatment-it’s to find the right balance. One that keeps you healthy without making you fall.
Because standing up shouldn’t feel like a gamble.
Can orthostatic hypotension go away on its own?
Yes, in many cases-especially if it’s caused by medication. When the offending drug is stopped or replaced, symptoms often improve within days to weeks. About 70-85% of medication-induced cases resolve with proper adjustment. But if the cause is nerve damage from diabetes or Parkinson’s, it’s less likely to fully go away. That’s why identifying the trigger matters.
Does drinking more water really help with dizziness on standing?
Absolutely. Low blood volume is a major contributor to orthostatic hypotension. Drinking 2-2.5 liters of water daily increases blood volume and helps maintain pressure when standing. One study showed patients who increased fluid intake had a 40% reduction in dizziness episodes. Avoid alcohol and excessive caffeine-they make dehydration worse.
Are compression stockings worth it for orthostatic hypotension?
Yes, especially for people who can’t stop their medications. Compression stockings (20-30 mm Hg pressure) help push blood back from the legs to the heart, reducing the drop in blood pressure when standing. Studies show they reduce dizziness in over half of patients. They’re not a cure, but they’re a simple, low-risk tool that works.
Can I still drive if I have orthostatic hypotension?
It depends. If you’ve had near-fainting or fainting episodes, driving is unsafe. Sudden dizziness while driving can lead to accidents. Many states require reporting medical conditions that affect driving safety. Talk to your doctor. If your symptoms are controlled with medication changes or compression stockings, you may be cleared to drive. But never drive if you’ve felt dizzy in the past week.
Why do some medications cause orthostatic hypotension and others don’t?
It’s about how they work. Drugs like alpha-blockers and antipsychotics interfere with the nerves that tighten blood vessels when you stand. Diuretics reduce blood volume. Opioids slow brain responses. Other meds-like ACE inhibitors or beta-blockers-can cause OH too, but less often. Newer drugs are being designed to avoid these effects. For example, ziprasidone causes OH in only 5-10% of patients, while clozapine affects 35-45%.
Is orthostatic hypotension the same as low blood pressure?
No. Low blood pressure (hypotension) is a general term. Orthostatic hypotension is a specific type that only happens when standing up. Someone can have normal blood pressure lying down but crash when they stand. That’s orthostatic hypotension. It’s not about how low your pressure is overall-it’s about how much it drops with movement.
Can young people get orthostatic hypotension from meds?
Yes, but it’s less common. Younger people usually have better autonomic function. But if they’re on multiple high-risk drugs-like opioids, antidepressants, or antipsychotics-or have underlying nerve issues, they can still develop it. Cases in people under 50 are rare but documented, especially with high-dose psychiatric meds.
How long does it take to see improvement after changing a medication?
It varies. For diuretics or alpha-blockers, improvement can happen within 24-72 hours. For antipsychotics or antidepressants, it may take 1-2 weeks as the drug clears from your system. Most patients report noticeable relief within one to two weeks after the change. If no improvement after three weeks, the cause may be something else.

jalyssa chea
November 16, 2025 AT 14:24ive been dizzy for months and no one ever said it could be my meds i just thought i was getting old lol
Gary Lam
November 17, 2025 AT 02:34so let me get this straight... we're telling grandpa to stop his blood pressure med so he doesn't pass out trying to pee... but then he dies from a stroke because his bp's too high? classic american medicine
also why is no one talking about how the FDA approves these drugs knowing they'll make people fall? 🤔
Peter Stephen .O
November 18, 2025 AT 18:49yo this is wild but also so real
my grandma was on 8 meds and kept falling-doc said 'you're just getting older' until we sat down with a pharmacist and found out half of them were making her dizzy as hell
we swapped out the quetiapine for ziprasidone and she went from needing a walker to walking the dog every morning
it's not magic-it's just stopping the stuff that's literally making you weak
ask your doc: 'which of these am i taking because i'm supposed to feel like crap?'
ps-compression socks are a game changer. don't knock 'em till you try 'em
Andrew Cairney
November 19, 2025 AT 09:59they don't want you to know this but big pharma makes billions off falls
every time you trip because your med drops your bp, they sell you a hip replacement, a hospital bed, and 3 new drugs to 'fix' the side effects of the first ones
it's a pyramid scheme wrapped in a white coat
they profit from your weakness
they know this happens
they just don't care
watch for the next ad: 'dizzy from your meds? try our new drug that treats dizziness caused by your other meds!' 🤡
vinod mali
November 20, 2025 AT 06:54i have seen this in my uncle in india too
he was on blood pressure and diabetes meds
he kept falling in bathroom
doc said nothing
we stopped hydrochlorothiazide and he was fine in 3 days
simple things matter
drink water
stand slow
ask questions
Jennie Zhu
November 20, 2025 AT 17:38the clinical significance of medication-induced orthostatic hypotension cannot be overstated, particularly within the geriatric population where autonomic dysregulation is prevalent. the 15-30% increased fall risk correlates strongly with elevated morbidity and mortality metrics, as evidenced by multiple longitudinal cohort studies. furthermore, polypharmacy constitutes a significant iatrogenic risk factor, with the odds ratio increasing exponentially beyond four concomitant agents. formal assessment via serial orthostatic vital signs remains the diagnostic gold standard, and pharmacologic intervention should be considered only after non-pharmacologic modalities have been optimized.
recommendations: hydration, compression garments, and timed ambulation protocols are first-line. midodrine may be indicated in refractory cases, though its alpha-1 agonist mechanism necessitates caution in supine hypertension.
Kathy Grant
November 22, 2025 AT 09:33there's something so deeply sad about how we treat aging
we give people pills for every little thing, then act shocked when they fall
we don't ask 'what is this person really needing?'
we just add another pill
it's like trying to fix a leaky roof by putting more tape on the inside
the real question isn't 'which drug is causing this?'
it's 'why are we giving so many drugs in the first place?'
what if we started with movement, food, connection, rest?
what if we trusted the body more than the bottle?
maybe the medicine isn't in the pill
maybe it's in the pause
the breath
the slow stand
the hand on the wall
Robert Merril
November 22, 2025 AT 12:45so you're telling me i shouldn't take my oxycodone and my zoloft and my lisinopril and my hctz all at once?
well damn
guess i'll just keep falling then
and yeah i typoed that last word
so what
you gonna write me a prescription for better spelling too?
btw my dr said 'it's just part of getting old' so i'm gonna keep doing what i'm doing
thanks for the info i guess
Noel Molina Mattinez
November 22, 2025 AT 19:42my dad took terazosin for 6 months and never said a word
he just kept saying 'i'm fine' until he cracked his skull on the tile
now he's got a plate in his head
and i'm still mad
why didn't anyone tell us?
why did they just keep giving him more pills?
they didn't care
they just wanted to check the box
Roberta Colombin
November 24, 2025 AT 17:59i think this is so important to share
many older adults feel embarrassed to say they get dizzy
they think it's normal
but it's not
it's a signal
and we owe it to our parents, our neighbors, our friends to ask
'have you been feeling lightheaded when you stand?'
it might save a life
thank you for writing this with care
Dave Feland
November 26, 2025 AT 10:26the real conspiracy here is that this information is buried under 17 pages of FDA-approved labeling and 37 clinical guidelines that no primary care physician reads
they're trained to prescribe, not to question
and the pharmaceutical reps? they don't mention the 32% increased mortality risk-they mention 'improved sleep' and 'reduced anxiety'
you think this is an accident?
no
it's systemic
it's designed
and you're being played
Ashley Unknown
November 27, 2025 AT 05:53have you ever wondered why all the people who get dizzy on meds are old?
why aren't the young ones getting it?
because they're not on the pills
and why aren't they on the pills?
because the system doesn't want them to be
the system wants you old
and broken
and dependent
and on 8 meds
so they can sell you the compression socks
the midodrine
the fall alarms
the hospital stays
the nursing homes
the grief counseling
they don't want you to stand up
they want you to sit down
and take your pills
and die quietly
they don't care if you live
they care if you consume
and i'm not crazy
just awake
Georgia Green
November 29, 2025 AT 00:48i'm a nurse and i see this every day
patients say 'i'm dizzy' and we assume it's age
but when we check orthostatics, boom-systolic drops 30 points
we always forget to ask about meds
just a reminder: if you're on more than 5 meds, ask for a med review
it's not a waste of time
it's life-saving
Christina Abellar
November 30, 2025 AT 14:58stand slow. drink water. talk to your doctor.
simple. free. life-changing.
Eva Vega
December 2, 2025 AT 05:24orthostatic hypotension secondary to pharmacotherapy represents a clinically significant autonomic dysfunction, particularly in the context of polypharmacy among the elderly. the diagnostic criteria, as referenced, are well-established within the American College of Cardiology and American Heart Association guidelines. the pharmacologic agents implicated-alpha-blockers, tricyclic antidepressants, antipsychotics-demonstrate well-documented effects on sympathetic tone and baroreceptor sensitivity. non-pharmacologic interventions, including volume repletion and mechanical compression, remain first-line, with midodrine reserved for refractory cases due to its potential for supine hypertension. routine screening in patients aged 65+ on ≥3 medications is strongly recommended.
jalyssa chea
December 2, 2025 AT 06:50you know what? i just told my mom to stop her doxazosin
she said 'but my dr said it's good for my prostate'
i said 'but you almost died in the shower'
she cried
then she said 'ok'
2 days later she didn't feel dizzy anymore
so yeah
just ask