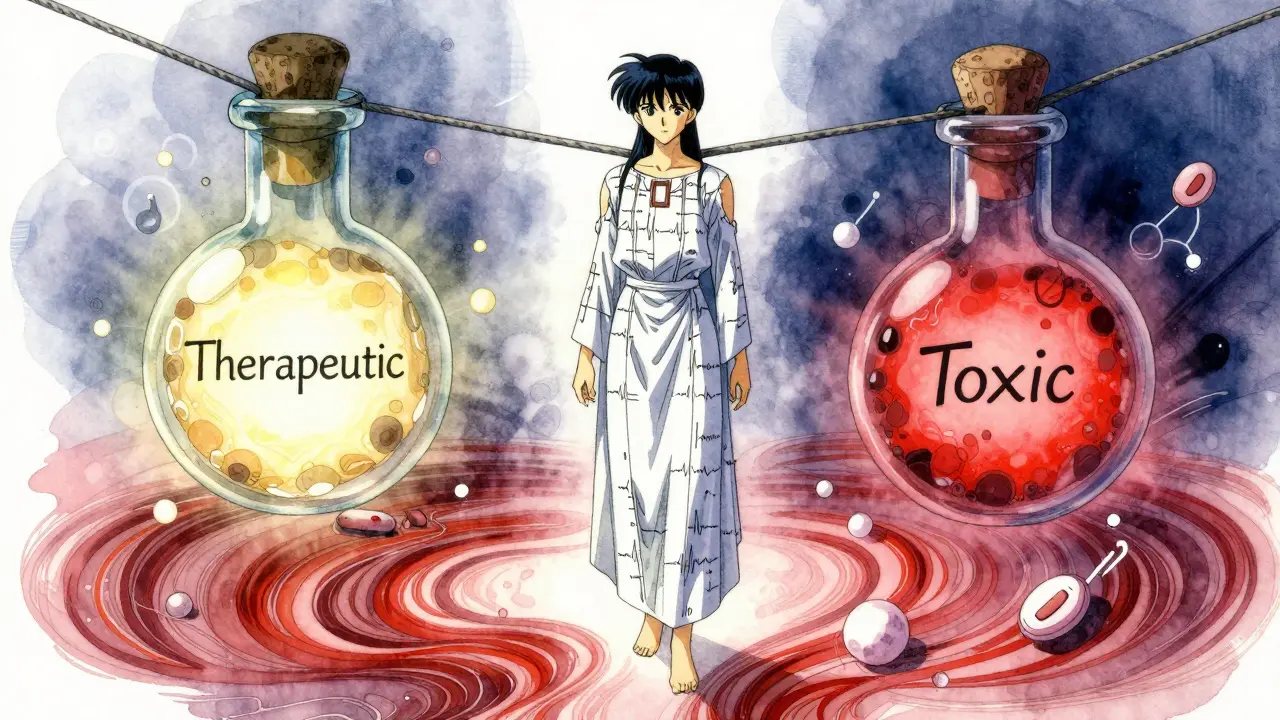
Some medications are like walking a tightrope. One tiny step too far, and things can go wrong-fast. These are called narrow therapeutic index drugs, or NTI drugs. They work wonders when dosed just right, but even a small change in amount can turn them from lifesavers into dangers. If you’re taking one of these, you need to know how they work, why they’re different, and what you must do to stay safe.
What Makes a Drug Have a Narrow Therapeutic Index?
Every drug has a range where it works without harming you. For most medicines, that range is wide. You can miss a dose or take it a little late, and nothing major happens. But with NTI drugs, that safe zone is razor-thin. The difference between the lowest dose that works and the lowest dose that causes harm is often less than double. That means if your blood level goes up just 10-20%, you could end up in the hospital.
Think of it like heating a pan. Too little heat, and your food stays raw. Too much, and it burns. With NTI drugs, the difference between perfect and dangerous is just a few degrees. For example, warfarin (Coumadin) keeps blood from clotting too much. The right level keeps you safe from strokes. But if your blood level gets too high, even a small bump-like a cut or fall-can cause serious bleeding. That’s why doctors check your INR regularly.
Common NTI Drugs You Might Be Taking
You might not realize you’re on an NTI drug. Here are the most common ones:
- Warfarin (Coumadin, Jantoven): Used to prevent blood clots. Must be monitored with blood tests (INR). Target range: 2.0-3.0. Above 3.5? Risk of bleeding skyrockets.
- Lithium (Lithobid): For bipolar disorder. Therapeutic range: 0.6-1.2 mmol/L. Above 1.5? Tremors, confusion, even seizures can happen.
- Levothyroxine (Synthroid): Replaces thyroid hormone. Even small changes in dose can make you tired, gain weight, or feel anxious. TSH levels must be checked every few months.
- Digoxin (Lanoxin): For heart failure and irregular heartbeat. Therapeutic range: 0.5-0.9 ng/mL. Above 2.0? Life-threatening heart rhythms can occur.
- Tacrolimus (Prograf): Used after organ transplants. Too low? Your body rejects the new organ. Too high? Kidneys get damaged. Levels are checked often, especially right after transplant.
- Phenytoin (Dilantin) and Carbamazepine (Tegretol): For seizures. Blood levels must be kept steady. Small changes can trigger seizures or cause dizziness, nausea, or even liver damage.
- Methotrexate (Trexall): Used for autoimmune diseases and some cancers. Too much can damage bone marrow and cause severe infections.
The FDA doesn’t publish an official list, but these are the drugs doctors and pharmacists agree are high-risk. If your doctor says you need regular blood tests to check your levels, you’re likely on an NTI drug.
Why Generic Switches Can Be Risky
Many patients switch from brand-name drugs to cheaper generics without thinking twice. But with NTI drugs, that’s not always safe.
Generic drugs must meet the same standards as brand-name ones. But for NTI drugs, the rules are stricter. The FDA now requires generic versions to be more tightly matched in how they’re absorbed by your body. While most generics can vary by up to 25%, NTI generics must stay within 90-111% of the brand’s absorption rate. That’s a huge difference.
Still, even small differences matter. A patient on warfarin switched from brand Coumadin to a generic. Within a week, their INR jumped from 2.5 to 4.1-dangerously high. They needed emergency treatment to stop the bleeding risk. Another patient on levothyroxine switched between two different generic brands and saw their TSH level swing from 1.8 to 8.4 in six weeks. That’s a huge shift in thyroid function-causing fatigue, weight gain, and brain fog.
Some states, like North Carolina, require pharmacists to get your doctor’s permission before switching your NTI drug to a generic. That’s because the risks are real. A 2021 study found patients who switched between different generic versions of NTI drugs were 2.3 times more likely to be hospitalized for complications.

Monitoring: Your Lifeline
There’s no way around it-if you’re on an NTI drug, you need regular testing. This isn’t optional. It’s how you stay alive and well.
- Warfarin: INR checks every 1-4 weeks, especially when starting or changing doses.
- Lithium: Blood tests every 3-6 months, or more often if your dose changes or you get sick.
- Levothyroxine: TSH and free T4 tests every 6-12 weeks after a dose change, then every 6-12 months if stable.
- Tacrolimus: Twice weekly at first after transplant, then monthly as you stabilize.
- Digoxin: Blood levels checked every few months, or if you feel dizzy, nauseous, or have irregular heartbeat.
These aren’t just routine visits. They’re your early warning system. Missing a test can mean missing a sign that your drug level is drifting into danger.
What to Watch For: Signs of Too Much or Too Little
You don’t need a lab test to know something’s off. Your body will tell you.
Too much (toxicity):
- Warfarin: Unexplained bruising, nosebleeds, blood in urine or stool, severe headaches.
- Lithium: Hand tremors, slurred speech, confusion, muscle weakness, frequent urination.
- Levothyroxine: Fast heartbeat, sweating, weight loss, anxiety, trouble sleeping.
- Digoxin: Nausea, vomiting, blurred vision, seeing halos around lights, irregular heartbeat.
Too little (underdosing):
- Warfarin: New swelling in legs, chest pain, sudden shortness of breath (signs of clots).
- Lithium: Return of mood swings, depression, or mania.
- Levothyroxine: Fatigue, weight gain, cold intolerance, dry skin, memory problems.
- Tacrolimus: Fever, joint pain, decreased urine output (signs of organ rejection).
If you notice any of these, call your doctor. Don’t wait. Don’t assume it’s just a bad day. With NTI drugs, symptoms can escalate fast.
How to Stay in Control
Managing an NTI drug isn’t just about taking pills. It’s about building habits that keep you safe.
- Stick to one pharmacy. They keep your history and can flag dangerous switches.
- Never switch brands without talking to your doctor. Even if the generic looks the same, it might not act the same.
- Keep a simple log. Write down your dose, when you took it, and any symptoms. Apps like Medisafe or MyThyroid can help track this.
- Watch for interactions. Grapefruit juice, certain antibiotics, and even some supplements can change how NTI drugs work. Ask your pharmacist before taking anything new.
- Bring your meds to every appointment. Your doctor needs to see exactly what you’re taking-bottle labels, not just names.
- Set reminders. Missed doses or late refills can throw off your levels. Use phone alarms or pill organizers.
Patients who track their meds and symptoms are 32% less likely to have serious side effects. That’s not a small number. It’s life-changing.
What’s Changing Now?
The field is getting smarter. In 2023, the FDA released new guidance for 15 specific NTI drugs, including levothyroxine and digoxin, with clearer rules for generics. Hospitals are now using barcode scanning on 12 high-risk NTI drugs to prevent dosing errors.
And the future is personal. Researchers are studying how your genes affect how you process these drugs. For warfarin, two genes (CYP2C9 and VKORC1) explain up to 60% of why people need different doses. By 2026, genetic testing may become standard before starting certain NTI drugs. That could cut adverse events by 35%.
These aren’t distant ideas. They’re happening now. And they’re making NTI drug therapy safer than ever-if you’re part of the process.
Final Thought: You’re Not Just a Patient-You’re a Partner
NTI drugs don’t care if you’re busy, tired, or forgetful. They react to your body, your doses, your habits. You can’t outsource your safety. But you don’t have to do it alone.
Work with your doctor. Talk to your pharmacist. Track your symptoms. Ask questions. If you’re unsure about a switch, a new pill, or a lab result-speak up. Your life depends on the details.
Many people on NTI drugs live full, stable lives. One Reddit user on r/BipolarReddit said, “Consistent lithium levels through regular blood tests has kept me stable for 8 years without hospitalization.” That’s not luck. That’s awareness. That’s control.
Are NTI drugs the same as high-risk drugs?
Yes, NTI drugs are a subset of high-risk medications. But not all high-risk drugs are NTI. NTI drugs are defined by their extremely narrow range between effective and toxic doses. Other high-risk drugs might be dangerous due to side effects, addiction potential, or interactions-but not necessarily because of tiny changes in blood levels.
Can I switch between generic brands of my NTI drug?
It’s not recommended without your doctor’s approval. Even small differences in how generics are made can change your blood levels enough to cause harm. If you must switch, your doctor should monitor your levels closely right after the change. Never switch on your own.
Do I need to take my NTI drug at the same time every day?
Yes. For most NTI drugs, timing matters. Taking warfarin at night, levothyroxine on an empty stomach, or lithium at the same time daily helps keep your levels steady. Irregular timing can cause fluctuations that lead to side effects or reduced effectiveness.
Why do I need blood tests if I feel fine?
You can feel fine even when your drug level is too high or too low. NTI drugs affect your body at a chemical level before you notice symptoms. Blood tests are the only way to know for sure your dose is still safe. Waiting until you feel bad could mean waiting too long.
Can I stop taking my NTI drug if I feel better?
Never stop without talking to your doctor. Stopping suddenly can cause rebound effects-like seizures with phenytoin, blood clots with warfarin, or mood crashes with lithium. Your doctor will guide you on how to taper safely, if needed.
Is there a list of all NTI drugs I can check?
The FDA doesn’t publish a public list. But your doctor or pharmacist can tell you if your medication is considered NTI based on clinical guidelines. Reliable sources like DrugBank and NIH’s StatPearls also identify them based on monitoring requirements and expert consensus.
Next Steps: What to Do Today
- Look at your current prescriptions. Do any of them match the list above?
- Check your last lab results. Are you on track, or are your levels drifting?
- Call your pharmacy and ask if your NTI drug has changed brands recently.
- Set a reminder for your next blood test-don’t wait for a letter.
- Download a free medication tracker app and start logging doses and symptoms.
NTI drugs demand attention. But with the right knowledge and habits, you can take them safely-without fear, without surprises, and with full control over your health.

Priscilla Kraft
January 11, 2026 AT 05:51Just started warfarin last month and this post literally saved my life 😭 I was about to switch to a generic because it was $20 cheaper... now I'm calling my doc to lock in the brand. Thank you for laying this out so clearly!
Alex Smith
January 12, 2026 AT 13:20Oh wow, so the FDA lets generics vary by 25%... unless you're on something that could kill you, then suddenly they care? 🤡 I'm sure the pharma execs are just sobbing into their yachts over this 'crisis'.
Madhav Malhotra
January 13, 2026 AT 18:56In India, we don't have this problem much because generics are the norm and doctors are super careful with monitoring. But I've seen people die because they switched brands without testing. This is a global issue, not just US.
Jason Shriner
January 14, 2026 AT 23:02so like... if i take my lithium at 7:01 instead of 7:00 am does my brain turn to mush? 🤔 i mean... we're talking about a 60 second window here. is that the line between enlightenment and emergency room? i'm just asking for a friend. (it's me.)
Alfred Schmidt
January 15, 2026 AT 04:20YOU'RE NOT SAFE. YOU'RE NEVER SAFE. YOU THINK YOU'RE DOING FINE? YOU'RE ONE BOTTLE OF GRAPEFRUIT JUICE AWAY FROM A BLOOD TRANSFUSION. YOUR PHARMACIST DOESN'T CARE. YOUR DOCTOR IS BUSY. YOU'RE ON YOUR OWN. STOP BEING LAZY.
Sean Feng
January 15, 2026 AT 04:26Why do we even need all this? Just take the pill. If you feel weird, stop. Simple.
Vincent Clarizio
January 16, 2026 AT 03:30Let’s be real - NTI drugs are the ultimate test of human frailty. We’re biological machines running on chemical equations written by nature, and we think we can tweak them like a smartphone app. But here’s the existential kicker: the difference between healing and harm isn’t a dosage - it’s a moment. A missed pill. A change in diet. A pharmacist’s decision. And we pretend we’re in control? We’re just guests in our own bodies, hoping the math doesn’t break down. That’s not medicine. That’s metaphysics with a prescription pad.
Sam Davies
January 16, 2026 AT 20:08Oh darling, you mean to tell me the FDA has *standards*? How quaint. I thought we were all just rolling the dice with our thyroid meds like it was a game of Russian roulette with a pill bottle. How terribly inefficient.
Christian Basel
January 16, 2026 AT 23:22Pharmacokinetic variability in NTI agents necessitates stringent therapeutic drug monitoring due to low therapeutic indices and nonlinear clearance profiles. Non-adherence to standardized dosing regimens correlates with increased incidence of adverse drug events (ADEs). Generic substitution without bioequivalence validation introduces unacceptable risk vectors.
Roshan Joy
January 17, 2026 AT 22:30My uncle takes lithium and he swears by his pill organizer + weekly blood tests. He says it's not about fear - it's about rhythm. Same time, same pharmacy, same logbook. He's been stable for 12 years. You don't need to be perfect, just consistent. 💪
Matthew Miller
January 18, 2026 AT 19:38Why are you all so emotional about this? This isn't a parenting blog. People die from meds every day. This is just one more. Get over it. Your anxiety isn't helping.