Imagine taking a pill because the label says "take daily", but you don’t know if that means once a day or every day. Now imagine you don’t speak English. This isn’t rare. It’s happening to millions of people in the U.S. every single day.
According to the U.S. Census Bureau, over 25 million people have limited English proficiency. That’s one in every 13 Americans trying to manage prescriptions in a language they barely understand. And the consequences? A 2006 Institute of Medicine report found these patients are 1.5 to 3 times more likely to have dangerous medication errors - from taking too much, too little, or the wrong drug entirely.
Why Translation Isn’t Just Helpful - It’s Life-Saving
Medication labels aren’t written for doctors. They’re written for patients. But most aren’t written in plain language - even for English speakers. For non-English speakers, they’re often impossible to understand.
Traditional pharmacy labels use medical jargon like "q.d." or "t.i.d." - Latin abbreviations that even some English-speaking patients don’t get. When translated by untrained staff or automated tools, these become worse. A 2020 FDA safety alert found automated translations had a 38% error rate in medication instructions. That means nearly two out of five translations were wrong.
But there’s a better way. The ConcordantRx project created simple, tested instructions in Chinese, Korean, and Russian that replaced medical terms with everyday language. Instead of "take one tablet by mouth twice daily", it said: "Take one pill each morning and each night". The result? 100% comprehension among tested patients. Compare that to just 45% with standard translations.
What Makes a Label Actually Understandable?
Good translation isn’t just about swapping words. It’s about clarity, culture, and context.
- Plain language: Instructions should be written at a 6th-grade reading level or lower. No medical terms. No abbreviations.
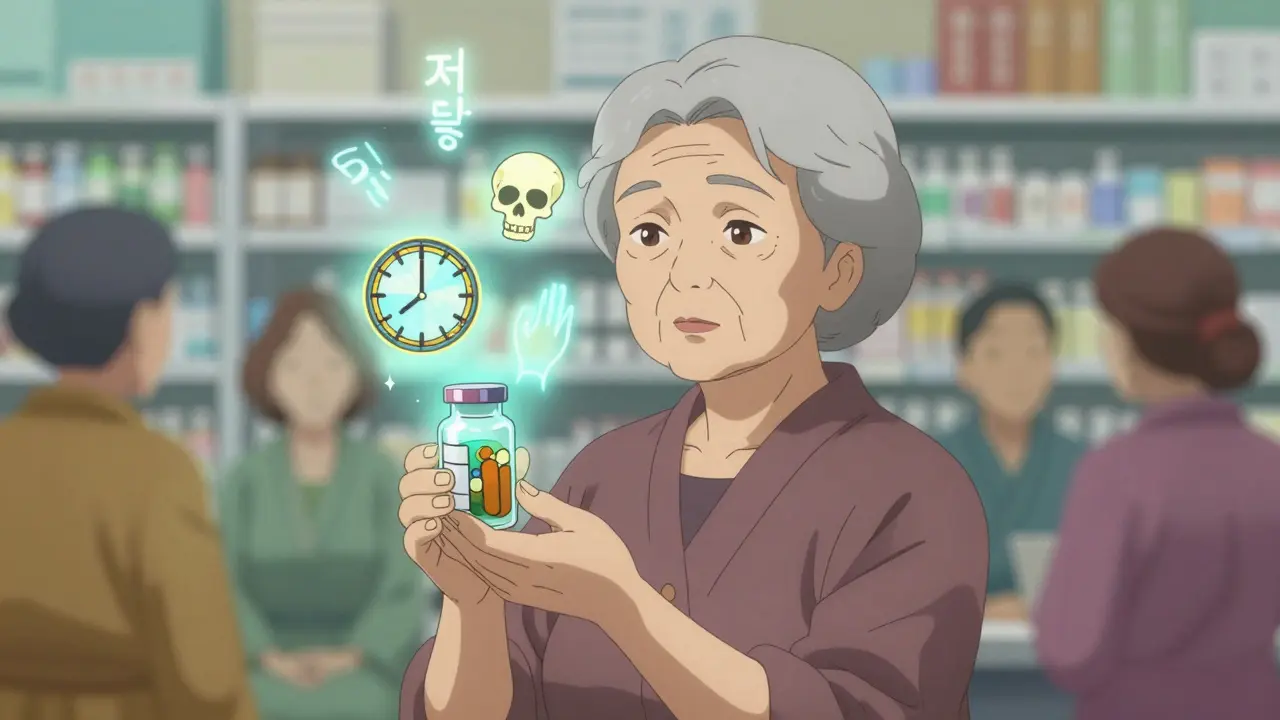
- Universal symbols: Icons approved by ISO 3864 and FDA guidelines - like a clock for timing, a skull for danger, or a hand holding a pill - help bridge language gaps.
- Visual aids: Pictures showing how to use an inhaler, inject insulin, or swallow a pill make instructions stick.
- Verbal confirmation: A professional interpreter doesn’t just translate - they ask, "Can you show me how you’ll take this?" to catch misunderstandings before they become emergencies.
A 2019 University of Michigan study showed that when pharmacies used this full approach - translated labels + interpreter + visuals - medication errors dropped by 58% and adherence improved by 37%.
Who’s Doing It Right?
Not enough pharmacies. Only 57% of community pharmacies in the U.S. offer translated prescription labels, according to a 2021 survey by the American Pharmacists Association.
But some are leading the way:
- RxTran offers FDA-compliant translations in 25 languages - including Amharic, Tagalog, and Somali - and integrates directly with pharmacy systems like Rx30 and PioneerRx.
- TransPerfect Healthcare and LanguageLine Solutions provide on-demand interpreter services and validated translations used in hospitals and large chains.
These services don’t just translate. They validate. Each instruction is reviewed by a medical translator who understands both the language and the medication’s purpose. They test comprehension with real patients before releasing labels.
Compare that to the common practice of asking a bilingual staff member - who may not know medical terms - to translate on the spot. A 2017 study found this method only worked 42% of the time.
The Cost of Cutting Corners
Some pharmacies avoid translation because they think it’s too expensive. Professional translation costs about $2.50 to $5.00 per prescription. But what’s the real cost of getting it wrong?
One case documented by WebM&M involved a patient who drank albuterol nebulizer solution because the bottle looked like a syringe - and the label didn’t say it wasn’t for swallowing. The patient ended up in the ER.
Another Reddit post from a pharmacist described a Korean patient taking a blood thinner twice a day because the label said "daily" - and they thought that meant "every day," not "once per day." That’s the kind of mistake that can cause a stroke.
The Institute for Safe Medication Practices found that using family members as interpreters leads to 65% higher error rates. Kids translating for parents. Neighbors guessing meanings. These aren’t solutions - they’re risks.
What the Law Actually Requires
It’s not optional. Under Title VI of the Civil Rights Act of 1964, healthcare providers receiving federal funds must give meaningful access to non-English speakers. That includes pharmacies.
Some states go further:
- California: Requires translation for the top 5 non-English languages spoken in each pharmacy’s service area. As of January 1, 2024, pharmacies must certify their language access process.
- New York City: Mandates translation for the top 10 languages.
- Federal Medicare Part D: Now requires plans to report on language access performance.
Yet, compliance is spotty. A 2022 California audit found 68% of pharmacies used outdated translations. Some still had labels from 2018.
What You Can Do - Whether You’re a Patient or a Pharmacist
If you’re a patient:
- Ask: "Can you give me my instructions in my language?" Don’t wait for them to offer it.
- Ask: "Can someone explain this to me in person?" Even if you get a label, verbal confirmation saves lives.
- Bring a friend or advocate who speaks both languages - but don’t rely on them alone.
- Check if your pharmacy has a multilingual website or app with audio instructions.
If you’re a pharmacist or staff member:
- Ask every patient: "What language do you prefer to talk about your medicine?" Write it down. Don’t assume.
- Use certified translation services - not Google Translate, not a bilingual cashier.
- Train your team on cultural competency. California requires 8 hours of training - every pharmacy should do it.
- Track comprehension. Ask patients to repeat back instructions in their own words. If they can’t, try again.
What’s Coming Next
The future is changing fast. In 2024, the Office of the National Coordinator for Health IT will require electronic health records to automatically detect a patient’s language preference and trigger translated instructions.
AI translation tools are being developed - but the FDA warned in 2023 that unvalidated AI tools still produce 43% error rates. That’s worse than using a human who doesn’t know medicine.
By 2026, experts predict 85% of pharmacies will have some form of language access system - not because it’s trendy, but because it’s proven to save money and lives. Pharmacies using full language services report 22% higher patient satisfaction and 15% lower costs from medication error-related visits.
The bottom line? Medication safety isn’t just about pills and doses. It’s about communication. And if you can’t understand your medicine, you can’t take it safely.
Frequently Asked Questions
Do pharmacies have to provide translated prescriptions by law?
Yes. Under Title VI of the Civil Rights Act, any pharmacy receiving federal funding - including those that bill Medicare or Medicaid - must provide meaningful access to non-English speakers. This includes translated prescription labels and access to professional interpreters. States like California and New York City have added stricter rules requiring translation for the top languages spoken in their communities.
Can I use Google Translate or my phone to understand my prescription?
No. A 2020 FDA safety alert found automated tools like Google Translate have a 38% error rate when used for medication instructions. Even if the translation looks right, it can miss medical context - like whether a drug should be taken with food, or if it interacts with another medication. Always ask your pharmacy for a professionally translated label or to explain it in person.
What if my language isn’t supported by my pharmacy?
If your language isn’t listed, ask if they can connect you to a live interpreter by phone or video. Many pharmacies use services like LanguageLine or TransPerfect that offer interpreters in over 200 languages - even rare ones like Hmong or Navajo. You can also request a printed translation be ordered. It may take a day or two, but it’s your right to understand your medication.
Why can’t my child or friend translate for me?
Family members often don’t know medical terms - like "hypertension" or "anticoagulant" - and may simplify or skip details out of fear or confusion. A 2022 report from the Institute for Safe Medication Practices found using untrained interpreters leads to 65% more medication errors. It’s safer to use a certified medical interpreter who understands both the language and the medical context.
How do I know if my prescription label is accurate?
Ask the pharmacist: "Can you show me how to take this?" Then, repeat the instructions back in your own words. If you’re unsure about the dose, timing, or purpose, ask again. Good pharmacies will welcome this. If they get frustrated, consider switching to a pharmacy that prioritizes clear communication - your safety matters more than convenience.
What’s Next for You
If you’re a non-English speaker, don’t wait for the pharmacy to help you. Ask for translation. Ask for a visual. Ask for someone to explain it - again if needed. Your life depends on it.
If you work in a pharmacy, start today. Add language preference to your intake form. Train your team. Partner with a certified translation vendor. You’re not just following the law - you’re preventing preventable harm.
Medication safety isn’t about how many pills you dispense. It’s about how many people understand them.

bob bob
January 5, 2026 AT 08:41Man, I never thought about how scary it must be to take medicine you don’t understand. My grandma took her blood pressure pill wrong for months because the label said 'once daily' and she thought that meant 'every day'-like, once per calendar day. She ended up in the hospital. This isn’t just about translation-it’s about survival.
Vicki Yuan
January 5, 2026 AT 15:37Finally, someone is talking about this properly. The FDA’s 38% error rate with automated translations is criminal. Plain language isn’t 'dumbing down'-it’s ethical design. If you can’t read it in six seconds, it’s not safe. I’ve trained pharmacy techs to use the ConcordantRx model. Results? 90% fewer calls to the hotline. Simple works.
Charlotte N
January 6, 2026 AT 10:14I’ve seen this happen at my local CVS… the girl behind the counter tried to translate my mom’s diabetes meds from Spanish using Google Translate… and she got the dosage wrong… I don’t even know how to feel about it…
Catherine HARDY
January 6, 2026 AT 21:19They say it’s about safety… but I think it’s about control. Why do they need to 'validate' translations? Why not just let people use their phones? Who’s really behind these 'certified' services? Who profits? The system doesn’t want you to understand-it wants you to depend.
saurabh singh
January 7, 2026 AT 06:14Bro in India we got this problem too. My aunt took her heart med twice because the label said '2 times' and she thought it meant 'two pills each time'-not 'two times a day'. No one taught her. No one checked. We need pictures, not just words. Even my 70-year-old uncle gets it when he sees a drawing of a pill with a clock.
Aaron Mercado
January 9, 2026 AT 01:30THIS IS WHY AMERICA IS FALLING APART!!! THEY’RE GIVING OUT MEDS LIKE CANDY AND NOT EVEN CHECKING IF PEOPLE KNOW WHAT THEY’RE TAKING!!! THE GOVERNMENT IS LETTING PEOPLE DIE BECAUSE THEY’RE TOO LAZY TO PRINT A FEW EXTRA LABELS!!! I SAW A WOMAN CRYING IN THE PHARMACY BECAUSE SHE COULDN’T READ HER ANTIBIOTIC LABEL-AND THE PHARMACIST JUST SMILED AND SAID 'YOU’LL FIGURE IT OUT'!!!
Vikram Sujay
January 9, 2026 AT 19:05The epistemological foundation of pharmaceutical communication rests upon the assumption of linguistic homogeneity-a assumption that, in multicultural societies, is not only untenable but ethically indefensible. The conflation of translation with comprehension constitutes a structural violence against epistemic marginalization. The solution, therefore, must transcend linguistic substitution and embrace semiotic inclusivity: iconography, oral confirmation, and participatory validation as constitutive elements of therapeutic justice.
Jay Tejada
January 11, 2026 AT 16:17So let me get this straight… we spend millions on AI that can’t even translate 'q.d.' right… but we still ask the 17-year-old cashier who just learned English last year to translate insulin instructions? Yeah… that’s a solid plan. 😅
Uzoamaka Nwankpa
January 12, 2026 AT 22:11My cousin died because she took the wrong pill. The label was in English. She didn’t speak it. No one helped. No one cared. Now I don’t trust any pharmacy. I don’t trust anyone who says 'it’s not their fault'.
Allen Ye
January 14, 2026 AT 17:49Consider the broader sociolinguistic implications: the medical-industrial complex has historically treated non-English-speaking populations as linguistic afterthoughts, reducing complex pharmacological regimens to binary translation tasks-ignoring cultural cognition, idiomatic nuance, and the embodied experience of illness. The ConcordantRx model doesn’t just translate-it re-ontologizes patient agency by centering lived understanding over lexical equivalence. This isn’t compliance-it’s decolonization of healthcare communication.
Shanna Sung
January 16, 2026 AT 01:27They’re hiding something. Why are only 57% of pharmacies doing this? Who’s paying them not to? I bet the drug companies don’t want patients understanding side effects. That’s why they push Google Translate. It’s all connected.
mark etang
January 16, 2026 AT 16:44As a licensed pharmacist with 22 years of experience, I can affirm that the implementation of validated, culturally competent language access protocols is not merely a regulatory obligation-it is a professional and moral imperative. The data presented is unequivocal. To neglect this standard is to violate the foundational tenets of patient safety and beneficence. I urge all institutions to adopt certified systems without delay.
Clint Moser
January 18, 2026 AT 05:19Look, the real issue is the FDA’s failure to standardize medical lexicon. 'q.d.' isn't the problem-it's that we still use Latin abbreviations in the 21st century. We need a unified pharmacological syntax, like ICD-11 for meds. Until then, all translations are just band-aids on a hemorrhage. Also, AI is fine if you train it on FDA-approved glossaries-Google Translate is garbage because it's trained on Reddit, not medical journals.
Enrique González
January 19, 2026 AT 13:51My brother’s a pharmacist in Chicago. He started using visual cards with icons for every med. Patients love it. Even if they don’t speak English, they nod and smile. One guy came back with a drawing he made of his pill schedule. He got it right. That’s the win. Not the label. The understanding.