Steroid Injection Risk Calculator
Steroid Exposure Calculator
Calculate your total steroid exposure from joint injections and identify potential risks based on current medical guidelines.
Your Steroid Exposure Assessment
Total Steroid Burden
Equivalent prednisone exposure (mg/year)
Risk Assessment
Recommended Actions
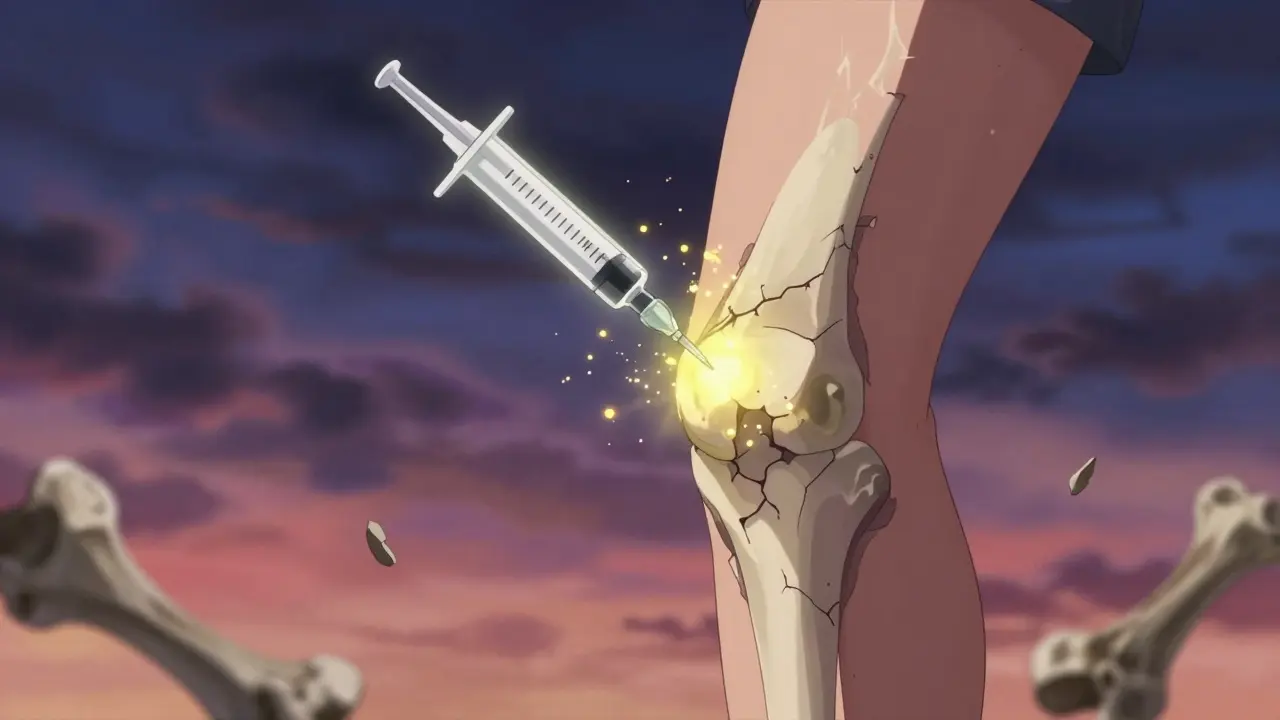
For millions of people with knee, hip, or shoulder pain, an intra-articular steroid injection has been a go-to solution. It’s quick, it’s common, and for many, it brings relief within days. But what if the shot that eases your pain is quietly doing harm to your joint-and your body? New research is turning long-held beliefs upside down. What we once thought was a safe, localized treatment is now showing signs of systemic damage, even when the needle never leaves the joint.
How Intra-Articular Steroid Injections Really Work
Intra-articular corticosteroid injections (IACS) deliver anti-inflammatory drugs directly into a joint. Common steroids used include triamcinolone acetonide, methylprednisolone acetate, and betamethasone. Doses vary from 10 to 80 mg, depending on the joint size. The idea is simple: reduce swelling and pain right where it hurts, without flooding your whole body with steroids.
It sounds perfect. And for decades, it was treated like a low-risk, high-reward tool. Over 12 million of these injections are given in the U.S. every year. But here’s the catch: steroids don’t stay put. Even when injected deep into the joint, some of the drug leaks into your bloodstream. That’s not a rare accident-it’s normal. A 2023 study in Radiology confirmed that systemic absorption happens in nearly all cases, especially with triamcinolone acetonide, which has one of the highest absorption rates.
The Hidden Damage: More Than Just Temporary Pain Relief
The real problem isn’t just what happens right after the shot. It’s what happens months or years later. Researchers at Boston University tracked over 1,000 patients who received hip and knee steroid injections. They found a 1% rate of serious joint damage: accelerated osteoarthritis, bone death (osteonecrosis), and stress fractures under the cartilage. That might sound small, but consider this: if 12 million injections are done annually, that’s 120,000 people at risk of permanent joint damage every year.
Another study from the Osteoarthritis Initiative found that people who got knee steroid shots were 3.2 times more likely to show visible joint space narrowing on X-rays over time. For those who got repeated injections, that risk jumped to 4.67 times higher. In hip injections, 44% of patients showed joint space narrowing within just six months.
This isn’t about a little cartilage wear. This is about structural collapse. The joint isn’t just aging-it’s being broken down faster than it should. And unlike natural osteoarthritis, which progresses slowly, this damage can accelerate rapidly after repeated injections.
Systemic Side Effects You Might Not Realize Are Connected
Even if your joint feels better, your body might be paying the price. Steroids that escape the joint can trigger real, measurable side effects across your system:
- High blood sugar: Especially dangerous for diabetics. Blood glucose can spike for days after the injection, sometimes requiring insulin adjustments.
- High blood pressure: Fluid retention and hormonal shifts can raise BP, even in people with no prior history.
- Bone loss: Corticosteroids suppress bone formation. Postmenopausal women are especially at risk for osteoporosis after repeated injections.
- Adrenal suppression: Your body stops making its own cortisol. This can lead to fatigue, low blood pressure, and even life-threatening adrenal crisis if you get sick or have surgery without proper steroid coverage.
- Cushing-like symptoms: Weight gain around the midsection, facial puffiness, thinning skin-these aren’t just side effects. They’re signs your body is being flooded with artificial steroids.
These effects aren’t rare. The American Journal of Roentgenology and the Cleveland Clinic both list them as documented risks. And they don’t vanish after a few days. Some last for weeks. That’s why doctors are now told to count every steroid injection-local or systemic-as part of your total steroid burden.

The Controversy: Why Some Doctors Still Say It’s Safe
Not everyone agrees. Some studies, like the one cited by the NIH in 2023, found no significant difference between steroid injections and placebo in terms of joint damage. Dr. Raynauld’s trial showed no joint space narrowing on X-rays. Dr. McAlindon found cartilage loss but no bone marrow lesions. So why the contradiction?
The answer lies in how we measure damage. Older studies looked at pain relief and X-rays. Newer ones use MRI, long-term follow-up, and precise joint space measurements. The truth is, cartilage loss can happen without causing immediate pain. You might feel better after the shot, but your joint is still deteriorating. That’s why some experts now say: “Just because you don’t feel worse doesn’t mean your joint isn’t getting worse.”
There’s also a financial and cultural inertia. Steroid injections are cheap, fast, and covered by insurance. Replacing them with physical therapy, weight management, or newer biologics takes time, resources, and patient education. So even as evidence mounts, the practice continues.
Who Should Avoid These Injections?
If you’re considering a steroid shot, ask yourself these questions:
- Are you under 50 with mild joint pain and no X-ray evidence of osteoarthritis?
- Do you have diabetes or high blood pressure?
- Are you postmenopausal or have a history of osteoporosis?
- Have you had more than two injections in the same joint in the past year?
- Is your pain worse than what your imaging shows?
If you answered yes to any of these, you’re in a higher-risk group. The Journal of the American Academy of Physical Medicine and Rehabilitation recommends extra caution for these patients. In fact, some experts now say: don’t give steroid injections to patients with early-stage osteoarthritis unless all other options have failed.
And if you’re planning surgery-like a knee replacement-steroid shots in the months before can increase your risk of infection and poor healing. Many orthopedic surgeons now refuse to operate on patients who’ve had recent steroid injections.
What Are the Real Limits? How Many Is Too Many?
Most guidelines say no more than 3 to 4 injections per joint per year. But that’s a guess. There’s no magic number that guarantees safety. The real limit is your total steroid exposure over time.
Think of it like this: every injection adds to your body’s steroid load. If you’re also taking oral steroids for another condition, that adds up fast. A single 40 mg triamcinolone shot can have the same systemic effect as 5 mg of prednisone for weeks. So if you’ve had three joint shots this year and you’re on 10 mg of prednisone daily, your total steroid burden is far higher than you think.
There’s no official tracking system. That’s why you need to keep your own record. Write down every injection: date, joint, drug name, dose. Bring it to every doctor visit. If you’re seeing multiple specialists, make sure they all know your full steroid history.
What Are the Alternatives?
If steroid shots aren’t the safe, simple fix we thought, what else works?
- Physical therapy: Strong evidence shows it’s as effective as steroids for knee osteoarthritis-and it builds joint strength without damage.
- Weight loss: Losing just 10 pounds reduces knee pressure by 40 pounds with every step. That’s more effective than any shot.
- Bracing and assistive devices: Simple knee braces or walking sticks can offload pressure and reduce pain.
- Hydrotherapy and low-impact exercise: Swimming, cycling, and tai chi improve mobility without pounding joints.
- Emerging treatments: Platelet-rich plasma (PRP) and hyaluronic acid injections are being studied as safer long-term options. Early data suggests less joint damage, though results vary.
None of these are instant fixes. But they don’t come with hidden risks. And over time, they often work better.
Final Thought: Pain Relief Isn’t Always Progress
We’ve been trained to think of pain relief as victory. But in joint health, it can be a trap. A steroid shot might silence your pain for a few months-but at the cost of your joint’s future. The goal isn’t just to feel better today. It’s to stay mobile, independent, and pain-free for years to come.
If you’ve had multiple steroid injections and still have pain, it’s not a sign you need more shots. It’s a sign your treatment plan needs a rethink. Talk to your doctor about the risks. Ask for imaging comparisons over time. Explore alternatives. Your joint doesn’t owe you quick relief. It deserves long-term care.
Can steroid injections cause long-term joint damage?
Yes. Multiple studies, including a 2023 study in Radiology, show that intra-articular steroid injections can accelerate osteoarthritis progression, cause subchondral fractures, and lead to osteonecrosis. This damage is often visible on imaging after repeated use, even if symptoms improve temporarily.
Do steroid injections affect blood sugar?
Yes. Steroids that enter the bloodstream can raise blood glucose levels for days after the injection. This is especially concerning for people with diabetes, who may need to adjust their medication temporarily. Monitoring blood sugar for 48-72 hours after an injection is recommended.
How many steroid injections are safe per year?
Most guidelines limit injections to 3-4 per joint per year. But the real limit is your total steroid exposure. Each injection adds to your body’s steroid burden. Patients with diabetes, osteoporosis, or those planning surgery should be especially cautious and may need fewer injections.
Are steroid injections safe for older adults?
They can be, but risks increase with age. Older adults are more likely to have osteoporosis, diabetes, or high blood pressure-all worsened by steroids. For older patients, non-drug treatments like physical therapy and weight management should be tried first. Injections should be reserved for cases where pain severely limits mobility and other options have failed.
What should I do if I’ve had multiple steroid shots and my pain is returning?
Don’t assume you need another injection. Return pain after multiple shots often signals that the joint is deteriorating faster than normal. Ask for updated imaging, review your steroid history with your doctor, and explore alternatives like physical therapy, braces, or weight loss. Continuing injections may speed up joint failure and make future treatments like surgery less effective.

Betty Bomber
January 26, 2026 AT 00:51Wow. I got my third knee shot last month and now I’m scared to even walk. My blood sugar’s been all over the place too. Guess I didn’t connect the dots.
Aurelie L.
January 27, 2026 AT 21:08They told me it was harmless. Now I’m reading this and realize I’ve been lied to.
Sally Dalton
January 29, 2026 AT 17:59I’m so glad someone finally said this. My mom had 5 shots in 18 months and now her hip’s basically dead. She’s in pain every day and no one told her the risk. 😔
Karen Droege
January 31, 2026 AT 13:06As a physical therapist who’s seen 200+ patients go from ‘steroid fix’ to ‘total replacement,’ let me tell you - PT doesn’t give you instant relief, but it gives you YEARS. I’ve had patients ditch shots and walk pain-free for a decade. It’s not sexy, but it’s real. 💪
SWAPNIL SIDAM
January 31, 2026 AT 14:03My uncle got 4 shots in one year. Now he can’t climb stairs. Doctors don’t care. They just give more shots. This is wrong.
Suresh Kumar Govindan
February 2, 2026 AT 08:18This is all part of the pharmaceutical agenda. Steroids are cheap, but the real profit is in joint replacements. They want you broken so they can fix you for $50K.
eric fert
February 2, 2026 AT 14:30Let’s be real - this article is fearmongering. I’ve had 7 steroid injections over 8 years. My knees still work. My blood sugar? Fine. My BP? Normal. My doctor’s been doing this for 30 years. You think he’s lying? Or are you just scared of anything that doesn’t come with a 12-step plan? 😏
Napoleon Huere
February 3, 2026 AT 04:36Isn’t it ironic? We treat pain like a bug to be eradicated, not a signal to be understood. The body isn’t broken - it’s begging for change. A shot silences the cry, but the wound remains. True healing isn’t about numbness. It’s about listening. 🌱
Allie Lehto
February 4, 2026 AT 21:56And yet… doctors still push these like candy. I had mine last week. My endo didn’t even ask if I was diabetic. Just ‘here, take this.’ They don’t care. The system is broken. 😭
Renia Pyles
February 6, 2026 AT 01:38Of course the system is broken. You think Big Pharma doesn’t fund the ‘safe’ studies? The NIH paper? Paid for by a pharma front. Wake up. They don’t want you healed. They want you hooked.
Faisal Mohamed
February 6, 2026 AT 19:43Epistemologically, the ontological assumption underlying IACS is predicated on a reductionist paradigm of joint pathology - yet emerging epigenetic and systemic biomarker data (e.g., IL-6, CRP spillover) suggest a holistic, networked inflammatory cascade that transcends anatomical boundaries. 🧬 Hence, the localized delivery fallacy is not merely a clinical oversight - it’s a metaphysical misalignment. 🤯
Dan Nichols
February 8, 2026 AT 01:24Studies show cartilage loss but not pain correlation. So what? If your X-ray looks worse but you feel better you’re winning. Stop overthinking. You don’t need a PhD to know when your knee stops hurting
Rakesh Kakkad
February 9, 2026 AT 20:13Respected medical authorities have long emphasized that intra-articular corticosteroid administration remains a cornerstone of conservative management in degenerative joint disease. The cited studies exhibit selection bias and lack long-term longitudinal control groups. I urge caution in interpreting preliminary data as paradigm-shifting. The clinical experience of millions contradicts the alarmist narrative.