Most kids get sick. A lot. A preschooler might have 8 to 12 colds a year. That’s normal. But when infections don’t stop, don’t respond to antibiotics, or keep getting worse, something deeper might be going on. Recurrent infections aren’t just bad luck-they can be the clearest sign of an underlying immunodeficiency. And catching it early can change everything.
When Is a Recurrent Infection a Red Flag?
It’s not about how many colds you get. It’s about the type, severity, and response to treatment. The American Academy of Allergy, Asthma & Immunology and the European Society for Immunodeficiencies have laid out clear warning signs that go beyond everyday illness.- Four or more ear infections in one year
- Two or more serious sinus infections in a year
- Two or more pneumonias within 12 months
- Persistent oral thrush after age 1
- Deep skin or organ abscesses that keep coming back
- Infections that don’t clear up after two months of antibiotics
- Need for intravenous antibiotics to treat infections
- Two or more deep-seated infections like septicemia or meningitis
- Failure to gain weight or grow normally
- Family history of primary immunodeficiency
These aren’t vague suggestions. They’re evidence-based thresholds. For example, oral thrush after age 1 has an 89% specificity for antibody deficiency. That means if a child still has white patches in the mouth past their first birthday, and it’s not tied to antibiotics or inhalers, it’s a major clue. Same with pneumonia-two in a year isn’t just a bad season. It’s a signal the lungs aren’t being protected properly.
What’s Really Going On? Beyond the Infections
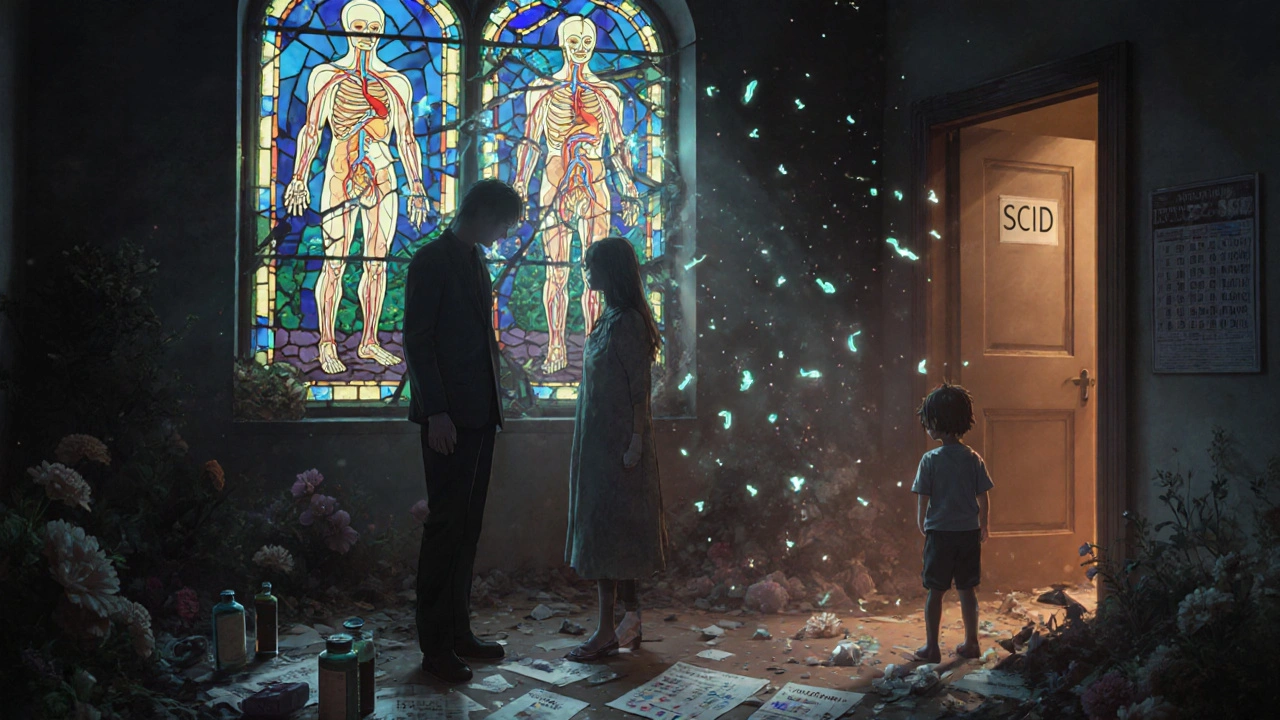
Physical signs matter just as much as infection history. A child with severe combined immunodeficiency (SCID) might have no tonsils or lymph nodes at all-78% of cases show this. Ataxia-telangiectasia, a rare disorder, often shows up as spider-like blood vessels on the skin and eyes. Growth failure is another silent red flag. Nearly two-thirds of children with undiagnosed immunodeficiencies fall below the 5th percentile for height and weight by age 5.And then there’s the type of germ causing the infection. If someone keeps getting infections from organisms that rarely harm healthy people-like Pneumocystis jirovecii, Cryptosporidium, or certain fungi-it’s a huge red flag. These are called opportunistic infections. They don’t just mean you’re run down. They mean your immune system isn’t even trying to fight back.
The Workup: How Doctors Test for Immunodeficiency
If these signs are present, the next step isn’t more antibiotics. It’s a structured diagnostic workup. It starts simple, then gets more specific.First: Complete Blood Count (CBC) with Differential
This basic test checks white blood cell counts. In kids over 1, a lymphocyte count under 1,500 cells/μL raises concern. In infants under 1, anything under 3,000 is a warning. Low lymphocytes mean the body’s frontline defenders are missing.
Second: Immunoglobulin Levels (IgG, IgA, IgM)
These are antibodies-the proteins that tag germs for destruction. But here’s the catch: normal levels change with age. A 6-month-old with an IgG of 558 mg/dL is fine. An 8-year-old with the same level? That’s dangerously low. Many doctors miss this. One pediatrician in Ohio told a story of three patients with CVID misdiagnosed because their IgG was 420 mg/dL-just above the old cutoff-but way below what’s normal for their age.
Third: Lymphocyte Subsets by Flow Cytometry
This test counts specific types of immune cells: CD3+ T cells, CD19+ B cells, CD56+ NK cells. If T-cell counts are under 1,000 cells/μL in a child over 2, it’s abnormal. This is how doctors spot SCID or DiGeorge syndrome before symptoms get catastrophic.
Fourth: Vaccine Response Testing
This is the gold standard. Giving a vaccine and checking if the body makes antibodies proves real immune function. For tetanus or diphtheria, a protective IgG level is ≥0.1 IU/mL. For pneumococcal vaccines, it’s ≥1.3 μg/mL. If a child gets a pneumococcal shot and their antibody levels don’t rise after 4-8 weeks? That’s not a bad vaccine. That’s a broken immune system.

Common Mistakes and What to Avoid
Too many patients get misdiagnosed. Too many get unnecessary treatments. Here’s what goes wrong:
- Calling transient hypogammaglobulinemia of infancy (common in 2-5% of babies) the same as CVID. Babies under 18 months often have low IgG as their immune system matures. Giving them IVIG too early does more harm than good.
- Missing secondary causes. Up to 30% of adults diagnosed with CVID actually have something else-like lupus, lymphoma, or side effects from medications like steroids or anti-seizure drugs.
- Ignoring anatomical problems. Forty-three percent of recurrent infection cases are due to physical issues: cystic fibrosis, chronic sinus blockages, or even a foreign object stuck in the airway. You don’t fix a blocked airway with immunoglobulin.
- Starting IVIG without proof of poor vaccine response. A 2020 study found 22% of patients got IVIG without ever having their antibody response tested. That’s not treatment. That’s guesswork.
What Happens If You Wait?
Delay isn’t just frustrating. It’s dangerous. In SCID, the most severe form of immunodeficiency, survival drops from 94% to 69% if diagnosis happens after 3.5 months of age. Why? Because without a functioning immune system, even a common virus can be deadly. By the time a child is hospitalized with pneumonia, sepsis, or meningitis, the damage is often irreversible.
Long-term, untreated antibody deficiencies lead to chronic lung disease, liver damage, and even cancer. CVID patients have a 20-fold higher risk of lymphoma. The longer you wait, the more your body pays.
What’s New in Testing?
Testing has gotten faster and smarter. In 2023, the FDA approved a next-generation gene panel called StrataID Immune that checks 484 immune-related genes in one test. It finds the genetic cause in 35% of suspected cases-double the rate of older methods. Some hospitals are already using it as a first-line test.
Meanwhile, newborn screening for SCID is now mandatory in 38 U.S. states, up from just 26 in 2018. That’s saving lives. Babies are being diagnosed before they get sick. In some places, the average time from suspicion to diagnosis has dropped from 9.2 years to just 2.1 years-thanks to better awareness and the 10 Warning Signs campaign by the Jeffrey Modell Foundation.
What Comes Next?
If testing confirms an immunodeficiency, treatment depends on the type. For antibody deficiencies like CVID or X-linked agammaglobulinemia, regular IVIG or subcutaneous infusions replace missing antibodies. For T-cell problems, bone marrow transplants can be curative. For rare syndromes, targeted therapies are now in clinical trials.
But the biggest win isn’t the treatment-it’s the diagnosis. Knowing what’s wrong ends the guessing. It stops the unnecessary antibiotics. It prevents hospitalizations. It gives families a plan. And in many cases, it gives children a future.
If you’ve seen a pattern of infections that don’t fit the normal story-deep, rare, stubborn, or life-threatening-it’s not just bad luck. It’s a message. Listen to it. Ask for the workup. Your immune system is trying to tell you something.
How do I know if my child’s infections are normal or a sign of immunodeficiency?
Normal infections in kids are mild, short-lived, and respond to standard care. Red flags include infections that are deep (like pneumonia or abscesses), recurrent (4+ ear infections/year), persistent (not clearing after 2 months of antibiotics), or caused by unusual organisms. If your child also has poor growth, chronic thrush after age 1, or a family history of immune problems, it’s time to ask for an immune workup.
Can adults have primary immunodeficiency too?
Yes. Many people live for decades with undiagnosed antibody deficiencies like Common Variable Immunodeficiency (CVID). Adults often present with chronic sinusitis, bronchitis, or pneumonia that won’t go away. Some are misdiagnosed with asthma or COPD. If you’ve had repeated lung infections, digestive issues, or autoimmune diseases along with infections, get tested. CVID is the most common antibody deficiency diagnosed in adults.
Is a low IgG level always a sign of immunodeficiency?
No. IgG levels change with age. A 6-month-old with 400 mg/dL is normal. An 8-year-old with the same level is not. Also, temporary drops can happen after viral infections or during growth spurts. The key is whether the low level is persistent and paired with poor vaccine response or recurrent serious infections. Always check age-adjusted reference ranges.
Do I need genetic testing to diagnose immunodeficiency?
Not always. Most cases are diagnosed with blood tests: CBC, immunoglobulins, lymphocyte subsets, and vaccine response. Genetic testing is used when the pattern suggests a specific inherited disorder-like SCID, X-linked agammaglobulinemia, or chronic granulomatous disease. It’s becoming more common as a second step, especially if initial tests are unclear.
Can immunodeficiency be cured?
Some can. Bone marrow transplants can cure severe T-cell deficiencies like SCID if done early. For antibody deficiencies like CVID, there’s no cure-but regular antibody replacement therapy (IVIG or SCIG) works extremely well to prevent infections and protect organs. The goal isn’t always a cure-it’s a normal life.
What should I ask my doctor if I suspect immunodeficiency?
Ask: "Could this be an immune problem?" Then request: a CBC with differential, IgG/IgA/IgM levels, lymphocyte subsets, and vaccine response testing. Don’t accept vague answers like "you’re just prone to illness." Ask for the specific thresholds used and whether levels are age-adjusted. If your doctor isn’t familiar, ask for a referral to an immunologist.


sharicka holloway
November 28, 2025 AT 08:52My niece had 5 ear infections in one year and we thought it was just bad luck. Then she stopped growing. Turns out she had CVID. IVIG saved her life. Don’t wait for the worst case scenario - if something feels off, push for the blood tests.
Savakrit Singh
November 29, 2025 AT 03:43Wow 😮 this is the most comprehensive breakdown I’ve seen. As a med student in India, I’ve seen so many kids with recurrent pneumonia dismissed as ‘weak immunity.’ This needs to be mandatory reading for every pediatrician here 🙏
Cecily Bogsprocket
November 29, 2025 AT 04:38I’ve been a pediatric nurse for 18 years, and I still get chills reading this. There’s a quiet tragedy in the kids who slip through the cracks - the ones labeled ‘fussy’ or ‘slow to grow’ while their immune system quietly collapses. This post doesn’t just inform - it gives parents permission to demand more. Thank you.
One thing I’ve learned: parents know their kids better than any lab. If a mom says, ‘This isn’t normal,’ she’s usually right. Trust that instinct - and then get the tests.
Alex Hess
November 29, 2025 AT 13:04Another overhyped medical article. ‘Two pneumonias in a year’? That’s statistically normal for kids in daycare. You’re pathologizing childhood. The real problem is overtesting and IVIG overprescription. This isn’t medicine - it’s fearmongering dressed up as science.
steve stofelano, jr.
November 30, 2025 AT 15:46As a physician practicing in rural Ohio, I’ve encountered multiple cases where IgG levels were misinterpreted due to outdated reference ranges. The case you referenced - a child with IgG at 420 mg/dL labeled ‘normal’ - is not anecdotal. It is systemic. We must update diagnostic criteria and educate frontline providers. This is not a niche concern; it is a public health blind spot.
Furthermore, the cost of delayed diagnosis far exceeds the cost of screening. The economic burden of recurrent hospitalizations, missed school days, and parental absenteeism is staggering. Prevention is not just medically sound - it is fiscally responsible.
Alex Hess
December 2, 2025 AT 00:23Oh please. You’re just another doctor trying to sell IVIG. My cousin got it for ‘low IgG’ and ended up with a blood clot. Your ‘science’ is just profit-driven panic.
sharicka holloway
December 2, 2025 AT 21:17My son got IVIG because his vaccine response was zero. He didn’t clot. He started playing soccer again. There’s a difference between reckless overuse and life-saving treatment. Don’t let one bad case scare you from real help.
Shubham Semwal
December 3, 2025 AT 19:28Bro, you’re telling me a kid with 4 ear infections needs a full immune workup? My cousin’s kid had 12 and still runs track. You’re overcomplicating normal childhood. Stop medicalizing everything.
sharicka holloway
December 4, 2025 AT 01:01That’s great for your cousin. But what if the kid had thrush after age 2 and never gained weight? Then it’s not ‘normal’ - it’s a red flag. One size doesn’t fit all.
Melania Rubio Moreno
December 5, 2025 AT 09:25u mean like… if u keep getting sick u might be sick? news at 11. 🙄
Emma Dovener
December 6, 2025 AT 20:32Just wanted to add - the StrataID Immune test is now available at major children’s hospitals in the US. If your pediatrician hasn’t heard of it, ask for a referral to a pediatric immunologist. It’s not sci-fi - it’s standard of care in 2024.
archana das
December 7, 2025 AT 23:32In India, we don’t have access to these tests. But I’ve seen mothers with no money, no doctors, just love - and they notice when their child stops smiling. Maybe the real test is not in the blood - but in the eyes of the mother who knows something’s wrong.
steve stofelano, jr.
December 8, 2025 AT 08:14Thank you for this perspective. Access to care is a global equity issue. While we advocate for advanced diagnostics, we must also empower caregivers with simple, clear warning signs - because sometimes, the first test is not in a lab, but in a mother’s intuition. That must be honored, validated, and supported - regardless of geography.