When you have inflammatory bowel disease (IBD) and you're thinking about getting pregnant, the biggest question isn't just can I get pregnant-it's can I stay safe while doing it. The fear of harming your baby with medications is real. But here's the truth: the biggest danger isn't the drugs-it's the disease itself. Uncontrolled Crohn's or ulcerative colitis during pregnancy raises your risk of preterm birth, low birth weight, and even stillbirth by more than double compared to women whose disease is in remission.
Why Stopping Medication Is Riskier Than Taking It
Many women with IBD stop their meds when they start trying to conceive, thinking they're protecting the baby. That’s the opposite of what you should do. A 2023 global consensus from 42 experts across 15 countries, backed by data from over 1,500 pregnancies tracked in the PIANO registry, found that women who stopped their IBD medications were far more likely to flare during pregnancy-and flares lead to complications.Think of it this way: if your IBD is active, your body is in constant inflammation mode. That stress affects your placenta, your nutrient delivery, and your baby’s growth. Medications that keep you in remission? They’re doing the heavy lifting so your body can focus on growing a baby.
Dr. Uma Mahadevan, who led the global guidelines, put it plainly: “Stopping medication leads to an increase in IBD symptoms, which can make pregnancies high-risk.” These aren’t high-risk patients because they’re pregnant-they’re high-risk because their disease isn’t controlled.
Medications That Are Safe to Keep Taking
Not all IBD drugs are created equal when it comes to pregnancy. Here’s what the latest evidence says:- Aminosalicylates (5-ASAs) like mesalamine and sulfasalazine are considered safe. The Crohn’s & Colitis Foundation recommends continuing them without change. But here’s the catch: if you’re on Asacol HD or another formulation with dibutyl phthalate (DBP) coating, switch immediately. DBP has been linked to genital malformations in male fetuses in animal and human studies. Lialda, Delzicol, and Apriso are DBP-free and safe alternatives.
- Anti-TNF drugs like infliximab (Remicade) and adalimumab (Humira) have the strongest safety record of any biologic. Over 2,000 pregnancies in the PIANO registry showed no increase in birth defects, preterm birth, or low birth weight compared to the general population. These drugs are often continued throughout pregnancy, though some providers may pause them in the third trimester to reduce drug transfer to the baby.
- Vedolizumab (Entyvio) is now considered safe based on data from over 100 pregnancies. Early concerns about lower live birth rates disappeared when researchers accounted for disease activity-meaning if you’re in remission, your chances of a healthy baby are just as good as with other safe meds.
- Ustekinumab (Stelara) data has grown rapidly. Over 680 pregnancies tracked by the manufacturer show no increased risk of birth defects or complications. A 2024 European study of 78 babies born to mothers on ustekinumab found no difference in outcomes compared to those on other safe treatments.
Medications to Stop Before Conception
Some drugs are simply too risky to take while pregnant-or even trying to get pregnant.- Methotrexate is a hard no. It’s a known teratogen and can cause severe birth defects in 17-27% of exposed pregnancies. If you’re on it, you need to stop at least 3-6 months before trying to conceive. Your doctor will switch you to azathioprine or another safe option.
- Thalidomide is banned during pregnancy worldwide due to its link to limb deformities. It’s rarely used for IBD, but if you’re on it, this is non-negotiable.
- JAK inhibitors like tofacitinib and upadacitinib are newer, and while early data looks promising (no birth defects in 11 pregnancies with tofacitinib), experts still recommend stopping them 1-6 weeks before conception. Why? Because they interfere with the JAK-STAT pathway, which plays a key role in early fetal development. Better safe than sorry.
What About Steroids?
Corticosteroids like prednisone are sometimes used to bring a flare under control. But they’re not a long-term solution-and they’re especially risky in the first trimester. Studies show a 1.4 to 2.3 times higher risk of cleft lip or palate when taken during early pregnancy. If you need steroids, use the lowest dose for the shortest time possible. Your goal should be to get off them before conception and stay off them with safer maintenance drugs.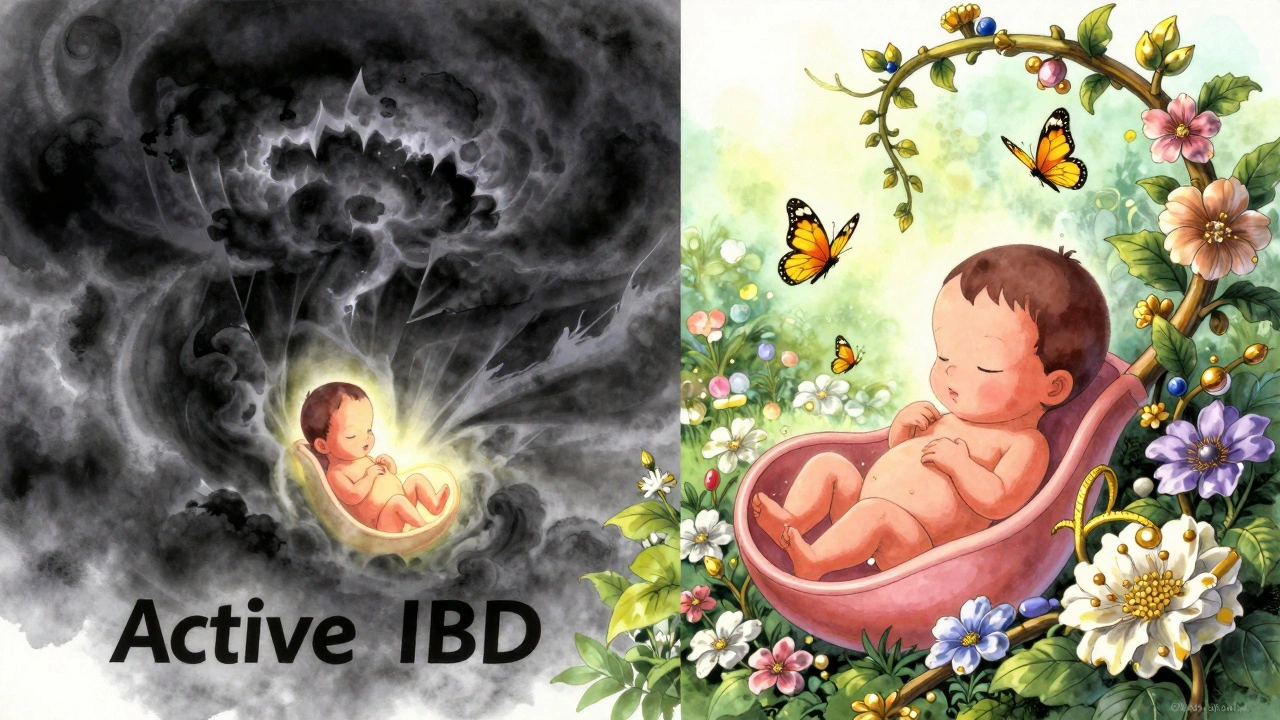
Immunomodulators: Azathioprine and 6-MP
Azathioprine and 6-mercaptopurine (6-MP) have been used safely in pregnancy for decades. Large studies show no increase in birth defects or developmental issues. The American College of Gastroenterology recommends continuing them through pregnancy, with regular blood tests to monitor your white blood cell count. These drugs cross the placenta, but the benefits of keeping your IBD quiet far outweigh any theoretical risks.What Happens After Delivery?
You might wonder: can I breastfeed while on my IBD meds? The answer is mostly yes.- 5-ASAs (mesalamine, sulfasalazine) are considered safe in breast milk. Even though sulfasalazine breaks down into sulfa, the amount passed to the baby is tiny and unlikely to cause harm.
- Anti-TNFs, vedolizumab, and ustekinumab are large proteins that don’t pass well into breast milk. Even if a trace amount does, it’s not absorbed by the baby’s gut.
- Immunomodulators like azathioprine are also considered compatible with breastfeeding.
- And yes-you can still give your baby all recommended vaccines, including live ones like MMR. Exposure to these drugs in utero doesn’t make vaccines dangerous.
Planning Ahead: The 3-Month Rule
The best time to talk about pregnancy isn’t when you miss your period. It’s 3 to 6 months before you start trying. This gives you time to:- Get your IBD into full remission-ideally confirmed by colonoscopy, not just symptoms
- Switch from unsafe meds (like methotrexate or DBP-containing mesalamine) to safe ones
- Start prenatal vitamins with extra folate (especially if you’re on sulfasalazine, which blocks folate absorption)
- Coordinate care between your gastroenterologist and OB-GYN
Too many women wait until they’re already pregnant to ask about meds. By then, you’re playing catch-up. The goal is to walk into pregnancy with your IBD under control and your meds already adjusted.

What If My IBD Flares During Pregnancy?
Flares happen-even with good planning. If you have a flare in the first trimester, don’t panic. The safest thing you can do is treat it aggressively with pregnancy-safe meds. Delaying treatment increases your risk of complications more than any medication ever could.Anti-TNFs and vedolizumab can be safely started during pregnancy if needed. Steroids may be used short-term, but again, only as a bridge-not a long-term fix. Your care team will monitor you closely, but remember: active disease is the enemy, not the medicine.
Where to Find Reliable Help
Not all doctors know the latest IBD and pregnancy guidelines. A 2021 survey found only 42% of community gastroenterologists could correctly identify all safe medications. Don’t assume your OB knows your IBD meds. Bring the PIANO guidelines with you-or print out the summary from the Crohn’s & Colitis Foundation.Ask for a joint appointment with your GI and OB. Many academic centers now offer specialized IBD pregnancy clinics. If yours doesn’t, request a referral. You deserve coordinated care.
The Bottom Line
You can have a healthy pregnancy with IBD. But it takes planning, the right meds, and the right team. The data is clear: continuing safe medications reduces your risk of complications more than stopping them ever could. Your baby’s safety isn’t about avoiding drugs-it’s about controlling your disease.Don’t let fear of medication stop you from becoming a parent. Let knowledge guide you instead.
Can I take mesalamine while pregnant?
Yes, but only if it’s a DBP-free formulation like Lialda, Delzicol, or Apriso. Avoid Asacol HD and other products with dibutyl phthalate coating, which have been linked to genital malformations in male fetuses. Mesalamine is one of the safest IBD medications during pregnancy and should be continued unless your doctor advises otherwise.
Is it safe to continue biologics like Humira or Remicade during pregnancy?
Yes. Anti-TNF biologics like adalimumab (Humira) and infliximab (Remicade) have been studied in over 2,000 pregnancies with no increase in birth defects, preterm birth, or low birth weight. Most experts recommend continuing them through pregnancy. Some may pause the last dose in the third trimester to reduce drug levels in the newborn, but this is optional and based on individual risk.
Should I stop my IBD meds if I’m trying to get pregnant?
No-not unless your medication is known to be harmful. Stopping safe meds like 5-ASAs, anti-TNFs, or azathioprine increases your risk of a flare, which is far more dangerous to your pregnancy than the medications themselves. Only stop drugs like methotrexate or JAK inhibitors, and only after talking to your doctor about safe alternatives.
Can I breastfeed while taking IBD medications?
Yes. Most IBD medications, including mesalamine, azathioprine, anti-TNFs, vedolizumab, and ustekinumab, are considered safe during breastfeeding. The amount that passes into breast milk is very low and not absorbed by the baby’s gut. You can safely give your baby all routine vaccines, including live ones like MMR.
What’s the biggest risk to my baby if I have IBD?
The biggest risk is uncontrolled IBD. Active disease at conception increases the chance of preterm birth by 2.3 times, low birth weight by 1.8 times, and stillbirth by 1.6 times. Medications used to control IBD pose significantly less risk than the disease itself. Keeping your IBD in remission is the single most important thing you can do for a healthy pregnancy.
When should I talk to my doctor about pregnancy and IBD?
At least 3 to 6 months before you start trying to conceive. This gives you time to get your disease into remission, switch to safer medications if needed, start prenatal vitamins, and coordinate care between your gastroenterologist and OB-GYN. Waiting until after you’re pregnant makes it harder to optimize your treatment safely.


Bee Floyd
December 1, 2025 AT 10:50Just read this whole thing and honestly? I wish my GI had told me this before I panicked and quit my meds. I went into my first trimester with a flare because I thought I was being "responsible." Turned out I was just being dumb. My daughter is 2 now, healthy as hell, but I still cringe thinking about how close I came to losing it all.
Don't let fear make the decisions. Let data. Let your team. Let your body breathe.
Also - DBP in mesalamine? That's wild. I had Asacol HD. Switched to Lialda after this. Zero regrets.
Jeremy Butler
December 2, 2025 AT 02:19The ontological implications of pharmacological intervention in reproductive physiology are profoundly complex. One must interrogate not merely the empirical outcomes of medication adherence, but the epistemic authority underpinning clinical guidelines derived from registries such as PIANO. The reductionist framing of risk as binary-medication versus disease-obscures the hermeneutic dimension of patient autonomy and the phenomenology of maternal anxiety.
That said, the preponderance of evidence does suggest that the cessation of immunomodulatory agents constitutes a greater threat to fetal homeostasis than their continuation, a conclusion that aligns with the Aristotelian principle of the mean: neither excessive fear nor reckless abandonment, but measured, evidence-based stewardship.
Courtney Co
December 3, 2025 AT 18:13I'm 32 and just found out I have Crohn's and I'm pregnant and I've been on methotrexate for 2 years and I just read this and I'm crying and I don't even know who to call and I'm scared I'm going to lose my baby and I didn't even know about the DBP thing and I took Asacol HD for 6 months and now I'm terrified and I don't know if I can switch in time and I'm so alone and why didn't anyone tell me this before I got pregnant and I hate that no one talks about this and I feel like I'm going to die inside.
Can someone please just tell me what to do?
Shashank Vira
December 4, 2025 AT 06:13How quaint. Western medicine, with its clinical trials and registries, presumes to hold the monopoly on truth. In India, we have centuries of Ayurvedic wisdom that recognizes the body as a dynamic equilibrium - not a machine to be dosed. Why are we so quick to trust pharmaceutical corporations over ancestral knowledge?
Have you considered turmeric? Ashwagandha? Panchakarma? The very notion that a biologic must be continued through pregnancy reveals a profound cultural arrogance - one that pathologizes the female body instead of harmonizing with it.
My cousin’s sister had IBD. She stopped all drugs. Ate organic, meditated, drank neem water. Delivered a healthy boy at 41. No drugs. No fear. Just dharma.
Eric Vlach
December 5, 2025 AT 15:52So many people don't realize that the real danger isn't the meds it's the flare
I had a friend who quit her Humira because she was scared and ended up in the hospital at 28 weeks with a perforation and her baby came at 30 weeks and spent 2 months in NICU
Just keep taking what your doctor says is safe
And if your doc doesn't know the guidelines find someone who does
Also mesalamine switch is huge I didn't know about DBP until last year
PS: breastfeeding is totally fine with all the safe meds don't let anyone tell you otherwise
Priyam Tomar
December 5, 2025 AT 19:06Oh please. This is just Big Pharma propaganda dressed up as science. The PIANO registry? Funded by AbbVie and Janssen. Of course they’re going to say anti-TNFs are safe. What else would they say?
And you want me to believe that injecting proteins into my bloodstream for 9 months won’t affect fetal development? That’s not science - that’s wishful thinking.
And don’t even get me started on "safe" breastfeeding. You think your baby’s gut doesn’t absorb anything? Tell that to the 12% of infants with immune dysregulation linked to maternal biologics.
There are no safe drugs. Only less dangerous ones - and even those come with hidden costs.
Irving Steinberg
December 7, 2025 AT 01:06Bro this is literally the most important post I’ve ever read 😭
I was about to quit my Humira because my mom said "meds are bad for babies"
Now I’m crying in my car at the gas station
Also DBP in Asacol?? That’s wild. I had that. I’m switching to Lialda tomorrow. No cap.
Also can we all just agree that steroids are the devil? 🙏
Also also - breastfeeding is fine?? YES. I was scared to nurse. Now I’m not.
Thank you. From the bottom of my heart. This saved me.
Lydia Zhang
December 8, 2025 AT 11:39My GI didn’t tell me any of this. I stopped everything. Flared. Preterm. NICU. Now I’m here.
Don’t be me.
Kay Lam
December 8, 2025 AT 23:44I’ve been living with ulcerative colitis for 17 years and I’ve had two pregnancies, both while on azathioprine and mesalamine, and both resulted in healthy children who are now 9 and 11. I want to say this because I know how overwhelming it is to be told you have to take drugs while pregnant - you feel like you’re poisoning your baby, even though you know logically that not taking them is worse.
What helped me was tracking my labs religiously, finding a GI who specialized in pregnancy, and joining a support group for IBD moms - not just any group, but one where people actually shared their lab values and medication schedules and hospital visits. It wasn’t about reassurance - it was about seeing real data from real people.
Also, the 3-month rule is non-negotiable. I didn’t follow it the first time. I got pregnant on a flare. It was hell. The second time, I waited. I got a colonoscopy. I switched meds. I took folate. I coordinated with my OB. And it was peaceful. I slept. I ate. I didn’t panic.
And yes - I breastfed both kids. No issues. No infections. No developmental delays. Just two happy, loud, messy toddlers who think their mom is weird because she has a stoma and talks about Crohn’s at the playground.
You can do this. But you have to plan. And you have to trust the science - not the fear.
Adrian Barnes
December 10, 2025 AT 04:58The entire premise of this article is dangerously naive. The PIANO registry is not a randomized controlled trial. It is observational data, subject to selection bias, confounding variables, and publication bias. Women who continue medications are more likely to be higher socioeconomic status, more educated, more compliant - factors independently associated with better pregnancy outcomes.
To attribute fetal safety to medication alone is to commit the ecological fallacy.
Furthermore, the long-term neurodevelopmental impacts of prenatal exposure to biologics remain unquantified. We have 2,000 pregnancies - but no 10-year follow-up studies. Where are the cognitive assessments? The autism rates? The immune profiling?
This is not medicine. This is marketing masquerading as guidance.
Linda Migdal
December 11, 2025 AT 20:49Let’s be real - if you’re on biologics and pregnant, you’re already privileged. Most women in this country can’t even afford to see a GI, let alone get a colonoscopy before conception.
And now you want them to switch from Asacol to Lialda? Lialda costs $1,200 a month without insurance.
This article reads like a pharmaceutical brochure for the 1%.
Meanwhile, my sister in Ohio is choosing between her meds and her rent. So don’t lecture me about "safe medications" when the system doesn’t make safety accessible.
Tommy Walton
December 13, 2025 AT 00:56So… the real villain isn’t the drugs.
It’s the fear.
And also, DBP in Asacol HD? That’s wild.
Also also - I’m doing this right now. Humira at 28 weeks. Breastfeeding. No worries.
Also also also - my baby’s got a full head of hair. Just saying. 🤓
James Steele
December 13, 2025 AT 19:43The ontogeny of maternal-fetal pharmacokinetics is often mischaracterized as a binary dichotomy: drug versus disease. Yet, the true paradigm lies in the nuanced interplay between placental transport dynamics, fetal cytochrome P450 expression, and the immunomodulatory threshold of gestational immune tolerance.
Anti-TNF agents exhibit placental translocation kinetics that peak in the third trimester - a fact often overlooked in clinical summaries. The decision to discontinue in late gestation is not arbitrary - it is pharmacodynamically informed.
Moreover, the assertion that "medications are safer than flares" assumes a homogenous disease phenotype - a fallacy. The heterogeneity of IBD, particularly in pediatric-onset cases, demands individualized risk stratification, not blanket recommendations.
Yet, we persist in reducing complex biology to bullet points. This is not medicine. This is algorithmic dogma.
Louise Girvan
December 14, 2025 AT 07:08Wait - so you’re telling me that the government and Big Pharma are hiding the truth about biologics and fetal development? And that the "safe" meds are just part of a larger agenda to normalize chemical dependency in mothers? And that the PIANO registry is funded by pharmaceutical companies that also own vaccine manufacturers? And that the CDC has been suppressing data on autism links since 2018?
I’ve been researching this for 3 years. I’ve read the whistleblower reports. I’ve talked to the mothers whose babies had brain bleeds after exposure.
Don’t take the drugs. Don’t trust the doctors. Go primal. Eat clean. Meditate. Your body knows what to do.
And if your baby gets sick? It’s not your fault. It’s the system’s.