Minocycline Tooth Discoloration Risk Calculator
Calculate Your Risk
Risk Results
Enter your information to see your risk level
Key Takeaways
- Minocycline is a broad‑spectrum tetracycline antibiotic that can treat certain gum infections, but it also carries specific oral side effects.
- When used correctly, it may reduce inflammation in periodontitis and help control aggressive bacterial growth.
- Common oral risks include tooth discoloration, gum irritation, and increased photosensitivity.
- Compared with other dental antibiotics, minocycline offers a longer half‑life but a higher chance of discoloration.
- Patients should discuss dosage, treatment length, and alternative options with their dentist or physician.
What Is Minocycline?
Minocycline is a semi‑synthetic tetracycline antibiotic first approved by the FDA in 1971. It works by inhibiting bacterial protein synthesis, making it effective against a broad range of gram‑positive and gram‑negative organisms. Because of its high lipid solubility, minocycline penetrates tissues-including inflamed gum tissue-more readily than some older tetracyclines.
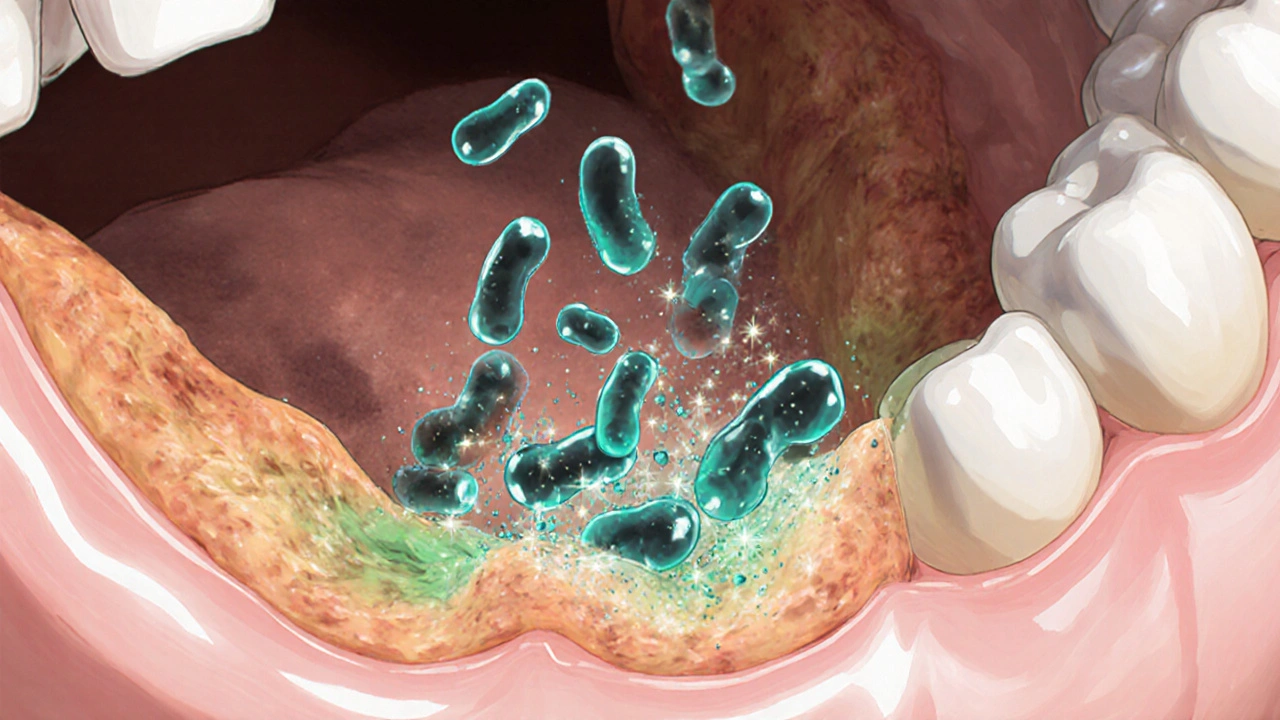
How Minocycline Works in the Mouth
When minocycline reaches the gingival crevicular fluid, it binds to bacterial ribosomes, stopping the production of essential proteins. This halts bacterial growth and reduces the inflammatory response that fuels gum disease. Its anti‑inflammatory properties also dampen matrix metalloproteinases, enzymes that break down collagen in the periodontal ligament.
Approved Uses vs. Off‑Label Dental Applications
Officially, minocycline is indicated for acne, certain respiratory infections, and rheumatic fever prophylaxis. Dentists sometimes prescribe it off‑label for aggressive periodontitis, peri‑implant infections, and as a component of local delivery systems (e.g., minocycline microspheres placed directly into periodontal pockets). The off‑label use is grounded in several clinical trials showing reduced pocket depth and improved attachment levels after a 2‑week systemic course.
Potential Benefits for Gum Disease
Recent studies (2023‑2024) indicate that a 14‑day course of 100 mg minocycline twice daily can lower the proportion of Porphyromonas gingivalis in chronic periodontitis patients by up to 70 %. The drug’s ability to concentrate in gingival tissues means it can reach bacteria that oral rinses miss. Patients also report less bleeding on probing and reduced gum swelling within a week of starting therapy.
Oral Side Effects You Should Know
While minocycline can be a powerful tool, it carries notable risks for dental health:
- Tooth discoloration: The drug can form pigmented complexes with calcium in developing teeth, leading to a gray‑blue hue. This is most common in children under eight but can affect adults with long‑term use.
- Gum irritation: Some patients experience a burning sensation or ulceration in the oral mucosa, especially at higher doses.
- Photosensitivity: Exposure to sunlight can cause oral tissue burns, so patients should avoid intense UV light during treatment.
- Antibiotic resistance: Overuse may select for resistant strains of Streptococcus mutans and other plaque bacteria, compromising future treatment options.
Comparing Minocycline With Other Dental Antibiotics
| Attribute | Minocycline | Doxycycline | Amoxicillin |
|---|---|---|---|
| Typical Dose (Adults) | 100 mg BID | 100 mg BID | 500 mg TID |
| Half‑Life | ≈ 11 h | ≈ 18 h | ≈ 1 h |
| Key Oral Benefits | High tissue penetration, anti‑inflammatory | Matrix metalloproteinase inhibition | Broad‑spectrum coverage |
| Risk of Tooth Discoloration | Moderate‑High | Low | None |
| Typical Resistance Concerns | ↑ Tetracycline‑resistant strains | Similar | β‑lactamase producers |
Practical Guidance for Patients and Dentists
- Assess the severity of periodontal disease. Minocycline is best reserved for moderate to severe cases where mechanical cleaning alone is insufficient.
- Consider patient age and dental development. Avoid systemic minocycline in children under eight or pregnant women unless absolutely necessary.
- Discuss dosage and treatment length. A typical 2‑week regimen balances efficacy with lower risk of discoloration.
- Advise on sun protection. Recommend sunscreen for lips and avoid tanning beds during therapy.
- Monitor for side effects. Schedule a follow‑up after one week to check for gum irritation or early signs of discoloration.
- Explore local delivery alternatives. Minocycline microspheres or gels placed directly into pockets can achieve high local concentrations with minimal systemic exposure.
Frequently Asked Questions
Can minocycline cause permanent tooth staining?
Yes, especially with prolonged use or in younger patients whose teeth are still forming. The discoloration can be difficult to reverse, so clinicians often limit the duration and dose.
Is minocycline more effective than doxycycline for gum disease?
Both belong to the tetracycline class and share similar antimicrobial spectra. Some studies suggest minocycline’s higher tissue penetration gives a slight edge in deep pockets, but the difference is modest.
What should I do if I notice my teeth turning gray while on minocycline?
Stop the medication immediately and contact your dentist or physician. Early discontinuation can prevent further staining, and professional whitening may mitigate existing hue.
Does minocycline interact with common dental products?
It can increase the photosensitivity effect of certain whitening gels containing peroxide. Avoid using strong whitening agents while on treatment.
Are there any alternatives for patients worried about side effects?
Yes. Options include local delivery of minocycline, systemic doxycycline (lower discoloration risk), or a short course of amoxicillin if the bacterial profile matches.
Understanding the balance between minocycline oral health benefits and its dental drawbacks helps patients and clinicians make smarter choices. When prescribed wisely, minocycline can be a valuable ally against stubborn gum infections, but vigilance for side effects remains essential.


Vikas Kumar
October 23, 2025 AT 16:38In India we see a surge of patients demanding quick fixes, and minocycline gets tossed around without proper dental supervision, which worries me because our healthcare system already struggles with antibiotic overuse, and the risk of tooth discoloration is especially concerning for children, so we need stricter guidelines and better public education.
Celeste Flynn
November 6, 2025 AT 15:38Minocycline can cause staining but you can lower the risk by using a short course and keeping good oral hygiene it also helps to brush after each dose and avoid coffee or tea during treatment using a straw for drinks can reduce contact with teeth and a regular dental checkup will catch any early discoloration before it becomes permanent
kenny lastimosa
November 20, 2025 AT 15:38When we examine the role of an antibiotic like minocycline in oral health, we are forced to confront the paradox of medicine: a tool that can both heal and harm. The pharmacodynamics tell us that its lipid solubility enables deep tissue penetration, which is a boon for battling periodontitis. Yet the same property also allows it to bind calcium in developing dentition, leading to the notorious gray‑blue hue. One might argue that the clinical benefits outweigh aesthetic concerns, especially in aggressive infections. However, the psychological impact of discolored teeth should not be dismissed lightly, as it can affect self‑esteem. Moreover, the emergence of tetracycline‑resistant bacterial strains poses a public health challenge that extends beyond the individual. The dentist’s decision to prescribe must therefore balance immediate therapeutic gain against long‑term microbial stewardship. Patients deserve a transparent discussion about dosage, duration, and alternative local delivery systems. In practice, many clinicians opt for a two‑week systemic regimen, hoping to limit exposure while still achieving periodontal improvement. Evidence suggests that pocket depth reduction can be significant within that window. Still, we must monitor for gum irritation, a symptom that often precedes more serious mucosal lesions. Sunlight exposure adds another layer of complexity, as photosensitivity can exacerbate oral tissue damage. The ethical dimension also surfaces when prescribing to younger patients whose teeth are still forming. Ultimately, the choice reflects a broader philosophical tension between intervention and restraint. By acknowledging both the pharmacological promise and the potential for collateral damage, we foster a more nuanced, patient‑centered approach.
Heather ehlschide
December 4, 2025 AT 15:38Great points about timing, I’d add that using a fluoride mouthwash after the course can help remineralize any early demineralization, and a professional cleaning midway through treatment can remove plaque that might otherwise harbor resistant bacteria.
Shubhi Sahni
December 18, 2025 AT 15:38Friends, when you consider minocycline, think about the whole picture, the benefits of deep tissue penetration, the risk of discoloration, the importance of patient age, the need for sun protection, and also the possibility of using localized microspheres, which can give high local concentration with minimal systemic exposure, so discuss all these factors with your dentist before starting therapy.
keerthi yeligay
January 1, 2026 AT 15:38I think short courses are ok but watch out for teath staining, also tell doc if you notice any orange hue early.
Peter Richmond
January 15, 2026 AT 15:38It is advisable to schedule a follow‑up appointment after one week of minocycline therapy to assess gum response, evaluate any signs of irritation, and adjust the treatment plan if necessary.
Bonnie Lin
January 29, 2026 AT 15:38Sounds good thanks
Tristram Torres
February 12, 2026 AT 15:38Using minocycline without checking is lazy.
Jinny Shin
February 26, 2026 AT 15:38Oh, the tragedy of teeth turned mauve!