Hepatitis C Drug Interaction Checker
Interaction Result
Blood Thinners
Warfarin, Rivaroxaban, Apixaban
Can increase bleeding risk when combined with DAAsStatin Medications
Atorvastatin, Simvastatin, Lovastatin
May cause muscle toxicity due to increased blood levelsAntacids & PPIs
Omeprazole, Pantoprazole, Aluminum/Magnesium Antacids
May reduce absorption of some DAAsSafety Tips:
- Always inform your healthcare provider about ALL medications you take
- Review your medication list with a pharmacist regularly
- Take DAAs exactly as prescribed
- Monitor for unusual symptoms or side effects
- Keep a medication diary during treatment
When dealing with Hepatitis C is a viral liver infection that can become chronic, leading to cirrhosis or liver cancer, the medication regimen you follow is as critical as the diagnosis itself. Modern cure rates exceed 95% thanks to direct‑acting antivirals (DAAs), but those drugs don’t work in isolation - they interact with many everyday prescriptions, over‑the‑counter remedies, and even certain foods. Hepatitis C drug interactions can lower cure odds, trigger side effects, or cause dangerous spikes in blood levels of other meds. This guide walks you through the most common interaction pitfalls, how to spot them, and what steps you can take to stay safe while clearing the virus.
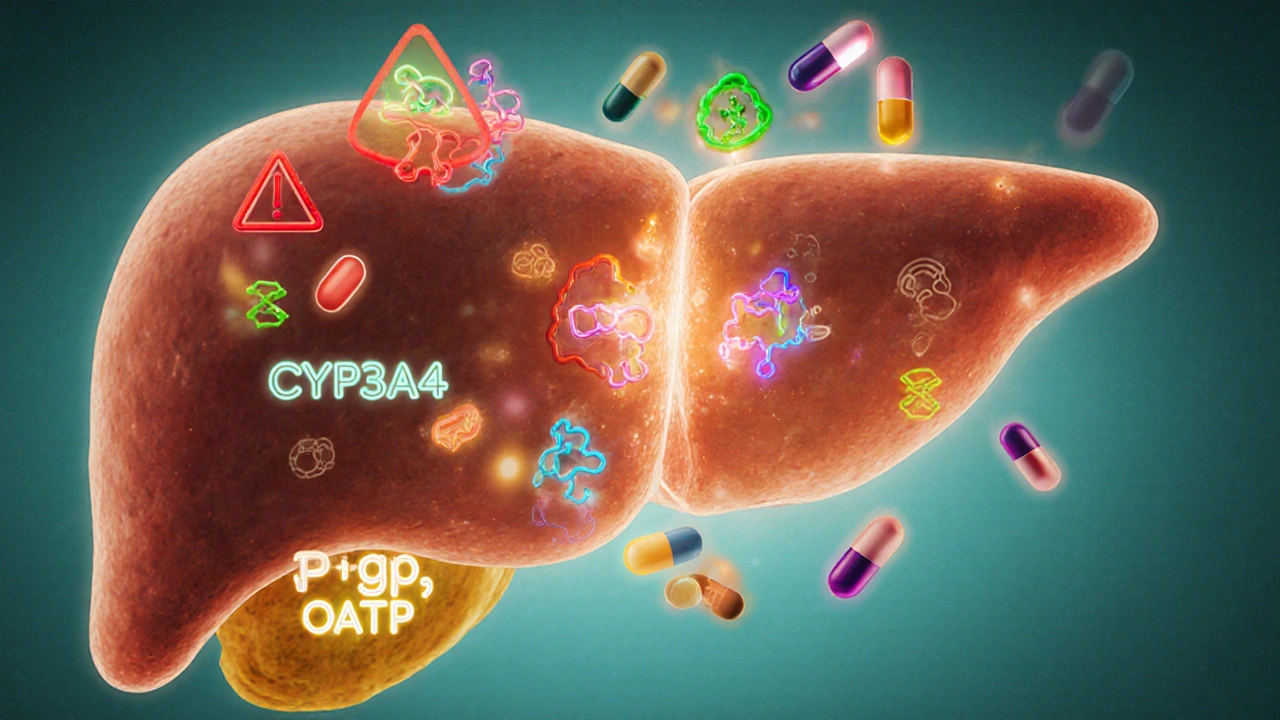
Why Drug Interactions Matter for Hepatitis C Treatment
DAAs are metabolized primarily by the liver’s cytochrome P450 (CYP) system, especially CYP3A4. Any drug that inhibits or induces these enzymes can alter the DAA’s concentration. Too low, and the virus may not be fully suppressed; too high, and you risk toxicity. Beyond enzymes, transport proteins like P‑glycoprotein (P‑gp) and organic anion transporting polypeptides (OATPs) also play a role. Because many chronic‑illness patients take multiple drugs (think cholesterol meds, blood thinners, or antidepressants), understanding the interaction landscape is essential for a smooth, successful cure.
Key Direct‑Acting Antivirals and Their Interaction Profiles
Below are the most frequently prescribed DAAs in the United States as of 2025. The first mention of each includes microdata markup so search engines can recognize them as distinct entities.
- Sofosbuvir is a nucleotide analogue that inhibits the HCV NS5B polymerase, used in combination regimens such as Harvoni and Epclusa. It is primarily excreted unchanged in the urine and has minimal CYP involvement, but it can be affected by P‑gp inhibitors.
- Ledipasvir blocks the HCV NS5A protein and is combined with sofosbuvir in Harvoni. It is a substrate of P‑gp and BCRP transporters, making it sensitive to drugs that affect these pathways.
- Glecaprevir is an NS3/4A protease inhibitor found in the pangenotypic regimen Mavyret (glecaprevir/pibrentasvir). It is metabolized by CYP3A4 and is a strong inhibitor of several transporters.
- Pibrentasvir is another NS5A inhibitor paired with glecaprevir. Like glecaprevir, it is processed via CYP3A4 and can interact with a wide range of drugs.
- Velpatasvir is the NS5A component of Epclusa (sofosbuvir/velpatasvir). It is a substrate for CYP3A4, P‑gp, and OATP1B1/1B3, creating a broader interaction potential.
Common Medication Classes That Can Clash with DAAs
Below is a practical checklist of drug families you should review with your prescriber or pharmacist before starting hepatitis C therapy.
| DAA | Key Metabolic Pathway | High‑Risk Interacting Drugs | Typical Management |
|---|---|---|---|
| Sofosbuvir/Ledipasvir | P‑gp, BCRP | Amiodarone, St. John’s Wort, Rifampin, Antacids with aluminum/magnesium | Adjust timing, avoid concurrently if possible |
| Glecaprevir/Pibrentasvir | CYP3A4, P‑gp, OATP1B1/1B3 | Erythromycin, Clarithromycin, Atorvastatin, Simvastatin, Carbamazepine | Switch to low‑interaction statin (e.g., pravastatin) or hold interacting drug |
| Sofosbuvir/Velpatasvir | CYP3A4, P‑gp, OATP1B1/1B3 | Warfarin, Amiodarone, HIV protease inhibitors, Anticonvulsants | Monitor INR closely, adjust dose, or substitute alternative agents |
Spotlight on High‑Impact Interactions
Warfarin is an oral anticoagulant that works by inhibiting vitamin K‑dependent clotting factors. When combined with certain DAAs, especially those that affect CYP3A4, warfarin levels can rise, leading to dangerous bleeding. If you’re on warfarin, your doctor will likely check your INR twice weekly during the first two weeks of hepatitis C treatment and adjust the dose accordingly.
Statins (e.g., Simvastatin, Atorvastatin) lower cholesterol by inhibiting HMG‑CoA reductase. Many DAAs inhibit the same transporters that move statins into liver cells, causing higher blood concentrations and a risk of muscle toxicity (myopathy). The safest approach is to switch to a statin with minimal CYP interaction, such as pravastatin or rosuvastatin, or to pause the statin for the 8‑12‑week treatment window.
Antacids and proton‑pump inhibitors (PPIs) can reduce the absorption of certain DAAs, most notably ledipasvir. If you rely on a PPI for reflux, ask your prescriber whether a timed‑dose separation (e.g., taking the DAA two hours before the antacid) or a switch to an H2 blocker is possible.
For patients with HIV, the overlap between hepatitis C DAAs and antiretroviral therapy (ART) is a common source of confusion. Some protease inhibitors (e.g., ritonavir‑boosted atazanavir) are strong CYP3A4 inhibitors and can dramatically increase DAA levels. In such cases, clinicians may adjust the ART regimen temporarily or select a DAA with a more favorable interaction profile, like sofosbuvir/velpatasvir.
Managing Interactions: Practical Steps for Patients
- Make a complete medication list. Include prescription drugs, over‑the‑counter pills, vitamins, herbal supplements, and any recreational substances.
- Consult a pharmacist. A pharmacist trained in hepatitis C can run a drug‑interaction check in seconds and flag any red flags.
- Schedule labs strategically. Baseline liver enzymes, renal function, and, when relevant, INR for warfarin should be drawn before starting therapy.
- Adjust timing. If a needed medication can’t be discontinued, spacing doses (e.g., taking the DAA in the morning and the interacting drug in the evening) often reduces the impact.
- Stay vigilant for side effects. New muscle pain, unexpected bruising, or changes in mental status should prompt an immediate call to your healthcare team.
- Document outcomes. Keep a simple log of any dosage changes, lab results, and symptoms throughout the 8‑12‑week course.
These steps keep the treatment on track and give your providers the data they need to intervene quickly if something goes off script.

Special Populations to Watch
Patients with advanced liver disease. Even though DAAs are generally safe, cirrhotic livers have altered drug metabolism. Dose reductions are rarely needed, but extra monitoring of bilirubin and albumin is advised.
Elderly patients. Age‑related declines in kidney function can affect sofosbuvir clearance. For patients over 75, checking creatinine clearance before prescribing sofosbuvir‑based regimens is standard practice.
Pregnant or breastfeeding women. Current guidelines recommend postponing DAA therapy until after pregnancy unless the disease is rapidly progressing, because safety data are limited. However, managing drug interactions remains crucial for any concurrent medications used during pregnancy.
Resources You Can Trust
Several reputable organizations maintain up‑to‑date interaction databases:
- The American Association for the Study of Liver Diseases (AASLD) provides a downloadable PDF of DAA interaction charts, refreshed yearly.
- Clinical Pharmacology’s interaction checker (access via most hospital portals) allows you to input multiple drugs and see real‑time alerts.
- World Health Organization (WHO) hepatitis C treatment guidelines include a section on managing co‑medications in low‑resource settings.
Bookmark these resources and refer back whenever you start a new medication. The effort pays off in a higher chance of achieving a sustained virologic response (SVR), which essentially means you’re cured.
Frequently Asked Questions
Can I take over‑the‑counter painkillers with hepatitis C meds?
Most NSAIDs such as ibuprofen are safe, but avoid high‑dose aspirin or certain COX‑2 inhibitors if you’re on a protease‑inhibitor DAA, as they can increase bleeding risk when combined with warfarin. Always check with your pharmacist.
What should I do if I miss a dose of my DAA?
Take the missed dose as soon as you remember, unless it’s less than 12hours before the next scheduled dose. In that case, skip the missed one and continue with your regular schedule. Missing more than two doses requires contacting your provider.
Do herbal supplements like milk thistle affect hepatitis C treatment?
Milk thistle and many other botanicals can induce or inhibit CYP enzymes. Because data are limited, most clinicians recommend stopping them during the 8‑12‑week DAA course.
Is it safe to drink alcohol while on DAAs?
Alcohol does not directly interact with DAAs, but it harms the liver and can slow recovery. Most providers advise limiting or abstaining from alcohol during treatment.
How often will I need blood work while on treatment?
Typical monitoring includes baseline labs, a repeat liver panel at week 4, and a final check at the end of therapy. Additional tests may be ordered if you’re on warfarin, have renal impairment, or are taking high‑risk interacting meds.

Brennan Keeler
October 7, 2025 AT 16:24Look, the DAA regimen ain't some vague suggestion, it's a rigorously engineered pharmacokinetic protocol. If you ignore the CYP3A4 interplay, you're practically inviting hepatic failure. The pharma guidelines are crystal clear: avoid P‑gp inhibitors unless you can offset timing. Warfarin interactions aren't optional, they demand weekly INR monitoring. And for the love of medicine, don't think a casual antacid will slip past the radar – the absorption hit can be catastrophic. Scope the interaction matrix before you even think about a dose.
Chelsea Hackbarth
October 9, 2025 AT 23:57💡Quick tip: always cross‑check your meds with a clinical pharmacist before starting Harvoni or Mavyret. The interaction check tool you posted is solid, but remember that over‑the‑counter NSAIDs can still tweak platelet function when combined with certain DAAs. Also, St. John’s Wort is a massive inducer – keep it off the list! 🙅♀️ And if you’re on a statin, pravastatin is usually the safest switch. 🌟
Adam Shooter
October 12, 2025 AT 07:30From an analytical standpoint, the pharmacodynamic landscape of direct‑acting antivirals (DAAs) is fraught with multilayered enzymatic interdependencies that demand exhaustive scrutiny. Firstly, the cytochrome P450 3A4 isozyme serves as a pivotal conduit for metabolic clearance, and any concomitant agent that functions as a potent inhibitor can precipitate supra‑therapeutic plasma concentrations of the antiviral agent, thereby amplifying the propensity for adverse events such as hepatotoxicity and QT‑prolongation. Secondly, transport proteins, notably P‑glycoprotein (P‑gp) and the organic anion transporting polypeptide family (OATP1B1/1B3), orchestrate hepatic uptake and efflux, meaning that inhibitors of these transporters can engender a cascade of bioavailability perturbations. Thirdly, the clinical ramifications of co‑administering warfarin with DAAs are non‑trivial; the ensuing pharmacokinetic interaction often manifests as an elevated International Normalized Ratio (INR), compelling vigilant monitoring protocols. Fourthly, statins, particularly simvastatin and atorvastatin, are susceptible to heightened plasma exposure due to competitive inhibition of metabolic pathways, predisposing patients to myopathic syndromes. Fifthly, acid‑suppressive therapies, such as proton‑pump inhibitors, attenuate the absorption of ledipasvir via alterations in gastric pH, thereby diminishing antiviral efficacy. Sixthly, the integration of antiretroviral therapy (ART) in co‑infected individuals introduces another stratum of complexity, with protease inhibitors like ritonavir exerting profound inhibitory effects on CYP3A4, which may necessitate dose adjustments or alternative DAA selection. Seventhly, herbal supplements, exemplified by St. John’s Wort, act as potent inducers of metabolic enzymes, potentially compromising therapeutic drug levels. Eighthly, the interplay between renal function and sofosbuvir clearance underscores the necessity for dose modification in patients with reduced creatinine clearance. Ninthly, the temporal spacing of medication administration can mitigate interaction severity; for instance, staggering DAA intake by several hours from a known inhibitor can attenuate peak concentration overlap. Tenthly, patient‑specific factors, such as age‑related pharmacokinetic changes, must inform individualized treatment plans to preempt suboptimal outcomes. Eleventhly, real‑world data consistently demonstrate that meticulous drug‑interaction surveillance correlates with higher sustained virologic response (SVR) rates. Twelfthly, the incorporation of multidisciplinary teams, including hepatologists, pharmacists, and infectious disease specialists, enhances the fidelity of interaction management. Thirteenthly, ongoing laboratory monitoring-encompassing liver function tests, INR, and creatine kinase-is indispensable to detect early toxicity signals. Fourteenthly, patient education regarding medication diaries fosters adherence and early detection of adverse effects. Finally, systemic adherence to evidence‑based interaction guidelines is the cornerstone of maximizing cure rates while safeguarding patient safety.
Shanmughasundhar Sengeni
October 14, 2025 AT 15:04Honestly, the interaction list looks like a parade of over‑hyped warnings. Most of the time, clinicians just knock off a statin for eight weeks and call it a day. The real culprits are the cheap over‑the‑counter pills that people think are harmless. If you’re still fumbling with antacids, just switch to an H2 blocker and move on. The guide is fine but could cut the jargon.
ankush kumar
October 16, 2025 AT 22:37Hey folks, just wanted to chime in with a friendly reminder that keeping a medication journal is a game‑changer. Write down every pill, supplement, and even the herbal teas you sip-some of those can mess with the DAAs in ways you didn’t expect. Also, don’t forget to check your kidney function before starting a sofosbuvir‑based combo, especially if you’re over 70. If you spot any weird bruising or muscle pain, it could be a statin interaction, so call your doctor ASAP. And yes, timing matters: take your DAA at least two hours apart from any P‑gp inhibitor if you can. Stay safe out there!
Cameron White
October 19, 2025 AT 06:10People don’t realize the government hides the real risks of these drugs.
Amélie Robillard
October 21, 2025 AT 13:44😂 Wow, love how everyone pretends they’re a pharmacology professor. Pro tip: if your doctor tells you to skip the antacid, just grab a gummy vitamin instead. 🍬 Seriously, the interaction tool is neat, but remember: no one’s perfect, so double‑check with a pharmacist!
Fae Wings
October 23, 2025 AT 21:17🫂 I totally get the anxiety about mixing meds-been there! The key is to keep an eye on any new aches or bruises and let your care team know right away. It’s like having a safety net; you’re not alone in this journey. 🌈
Anupama Pasricha
October 26, 2025 AT 03:50Supporting you all-remember that consistency is king. If you notice a pattern of side effects after a particular supplement, pause it and see if things improve. It’s a small step that can make a big difference in treatment success.
Bryce Charette
October 28, 2025 AT 11:24Just a quick grammar note: it's "warfarin" not "warfarin's" when you refer to the drug itself. Also, "monitor" should be paired with "your" for clarity, e.g., "monitor your INR levels." Keep the sentences concise; it helps everyone follow the regimen.
Christina Burkhardt
October 30, 2025 AT 18:57Great point about the medication diary! Adding timestamps to each entry can help you and your provider spot trends faster. If you ever feel uncertain, a quick call to your pharmacy can clarify potential interactions before they become an issue.
liam martin
November 2, 2025 AT 02:30In the grand theatre of life, we are but actors fumbling with scripts written by unseen hands. Yet, the very act of questioning the script-of probing the drug interactions-grants us a modicum of agency amidst the chaos.
Ria Ayu
November 4, 2025 AT 10:04Indeed, reflection brings clarity. By staying mindful of each medication’s story, we craft a harmonious narrative where treatment succeeds without unintended discord.
maya steele
November 6, 2025 AT 17:37To formalize the earlier suggestions: it is advisable to maintain an exhaustive ledger of all pharmacological agents, including herbal supplements, and to schedule periodic laboratory assessments-particularly liver function tests and coagulation profiles-throughout the therapeutic course.
Sharon Lax
November 9, 2025 AT 01:10The interaction chart is useful, but often clinicians overlook the subtleties of patient adherence when multiple drugs are involved. A holistic approach that accounts for lifestyle factors can mitigate many of these risks.
paulette pyla
November 11, 2025 AT 08:44Frankly, most of these guidelines are just corporate fluff to keep pharma’s profit margins high. If you’re truly smart, you’ll bypass the statins altogether and rely on diet instead.
Benjamin Cook
November 13, 2025 AT 16:17Hey team!!! Remember, consistency is key!!! 📅 Set alarms!!! Keep your meds organized!!! And if anything feels off-don’t wait!!! Call your provider RIGHT AWAY!!!
karthik rao
November 15, 2025 AT 23:50While the interaction matrix appears comprehensive, a meticulous audit reveals redundancies: certain CYP3A4 inhibitors are listed despite negligible clinical relevance at therapeutic doses. 📊 Hence, a stratified risk assessment is preferable to a blanket prohibition.