Every year, Americans spend over $650 billion on prescription drugs. That’s more than any other country in the world. But here’s the surprising part: generics make up 90% of all prescriptions filled - and yet they only account for 12% of total spending. Meanwhile, brand-name drugs, which make up just 10% of prescriptions, eat up 88% of the bill. This isn’t a glitch. It’s the system working the way it was designed to - and it’s saving patients, insurers, and taxpayers hundreds of billions every year.
How Generics Slash Prices - And Why It Matters
When a brand-name drug’s patent expires, any manufacturer can apply to make a generic version. The FDA doesn’t require them to repeat expensive clinical trials. Instead, they prove the generic is bioequivalent: it delivers the same amount of active ingredient into the bloodstream at the same rate as the original. That’s it. No need to prove it works again. Just prove it behaves the same way in the body. The result? Generics typically cost 80-85% less than the brand. A $350 monthly insulin prescription becomes $25. A $1,200 heart medication drops to $180. For people on fixed incomes, this isn’t just savings - it’s access. In 2024 alone, generics saved the U.S. healthcare system $98 billion in direct spending. That’s more than the entire annual budget of the CDC. The numbers don’t lie. In 2023, generic drugs saved $445 billion cumulatively. That’s the equivalent of covering health insurance for 15 million people for a full year. And it’s not just about pills. Generics cover everything from blood pressure meds to antidepressants to antibiotics. If you take a daily pill for a chronic condition, odds are it’s a generic - and you’re paying a fraction of what you would’ve paid a decade ago.The Hatch-Waxman Act: The Secret Weapon Behind Generic Access
None of this would exist without the 1984 Hatch-Waxman Act. Before this law, drug companies could keep prices high indefinitely by blocking competitors. Generic manufacturers had to start from scratch - running full clinical trials, which cost millions and took years. The result? Almost no generics existed. Hatch-Waxman changed that. It created a fast-track approval process called the ANDA - Abbreviated New Drug Application. It also gave brand-name companies a limited extension on their patents if they had to conduct new studies for safety changes. In return, generic makers got a 180-day exclusivity window to be the first to enter the market after patent expiry - a huge incentive. This wasn’t just a policy tweak. It was a revolution. Within 10 years, generic use jumped from 19% to over 50%. Today, it’s 90%. And the FDA now approves more than 1,000 new generic drugs every year. The system isn’t perfect, but it’s one of the most successful public health policies in modern American history.Generics vs. Biosimilars: The Next Frontier
Not all drugs are created equal. Simple chemical pills - like metformin or atorvastatin - are easy to copy. But biologics? Those are complex proteins made from living cells. Think insulin, rheumatoid arthritis drugs, or cancer treatments. You can’t just reverse-engineer them. That’s where biosimilars come in. Biosimilars aren’t exact copies. They’re highly similar versions. The FDA requires them to show no clinically meaningful differences in safety, purity, or potency. But because they’re harder to make, they don’t drop prices as dramatically. While generics save 80-85%, biosimilars typically save 15-35%. Still, that’s huge when you’re talking about drugs that cost $10,000 a month. The problem? Adoption is slow. In Europe, 70-85% of biologics prescriptions are filled with biosimilars. In the U.S., it’s only 25-30%. Why? Pharmacy benefit managers (PBMs) often push brands because they get bigger rebates. Doctors are hesitant because they’re not trained on biosimilars. And patients? Many still think “generic” means “inferior.” The FDA’s Biosimilars Action Plan aims to fix this. But with 90% of biologics set to lose patent protection in the next decade, and almost none having biosimilars in development, we’re heading for a crisis. If nothing changes, we’ll face massive spikes in drug spending - just as more seniors need these drugs.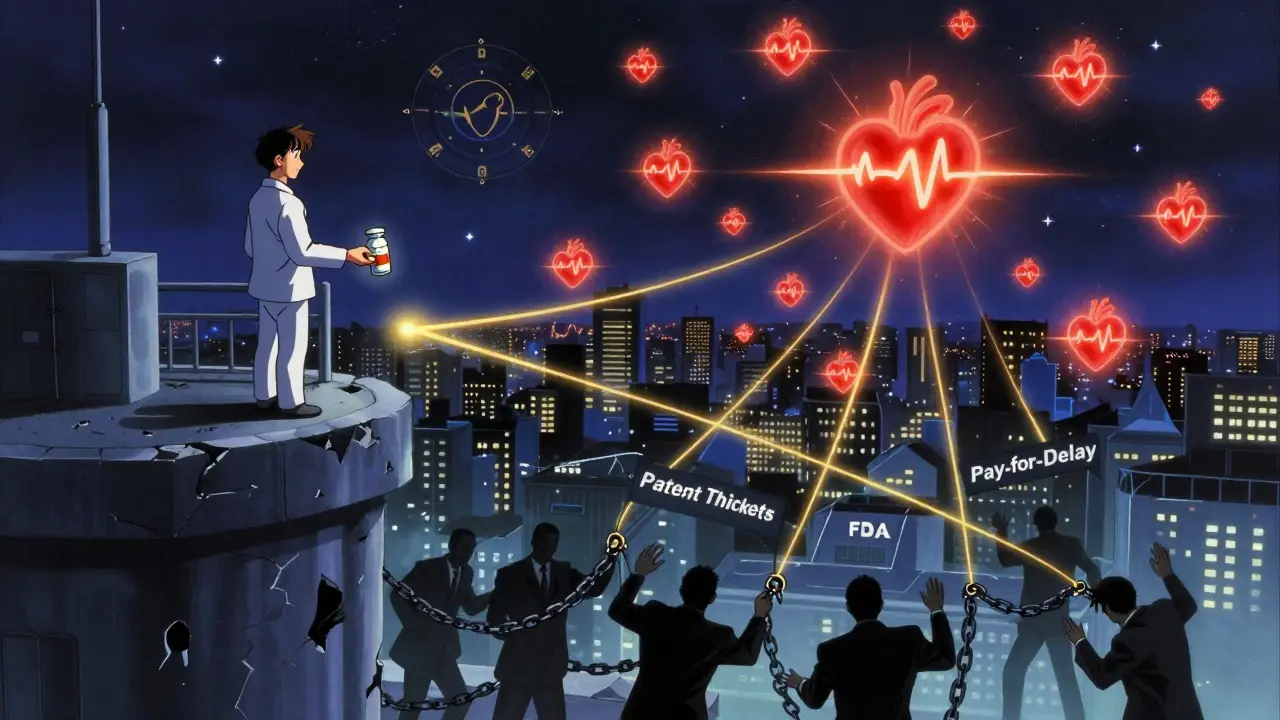
Why Some Generics Still Cost Too Much - And What’s Holding Them Back
You’d think with 90% of prescriptions filled with generics, prices would keep falling. But that’s not always the case. Sometimes, a drug’s price spikes - even after generics enter the market. Why? Three big reasons:- Patent thickets: Brand companies file dozens of minor patents on packaging, dosing schedules, or inactive ingredients. These don’t protect the drug itself - but they delay generics. One drug had over 140 patents. The average is 30-50. Each one adds months - sometimes years - to generic entry.
- Pay-for-delay deals: Sometimes, brand companies pay generic makers to stay away. The FTC found these agreements delay generic entry by 17 months on average. That costs consumers $3.5 billion a year in higher prices.
- Authorized generics: Brand companies sometimes launch their own generic version - under a different label - right when the patent expires. This keeps prices high because there’s no real competition. Instead of one generic at $20, you get the brand’s generic at $25 and no other options.
Real People, Real Savings - And Real Frustrations
Behind every number is a person. One Reddit user shared how switching her mom from brand-name Humalog insulin to generic insulin lispro cut the monthly cost from $350 to $25. That’s $325 saved every month. Without it, she would’ve had to choose between insulin and groceries. GoodRx data shows 68% of patients skip or split pills when generics aren’t available. That’s not laziness. That’s survival. For Medicare Part D beneficiaries, 42% reported skipping doses because of cost - but only 12% did so with generics. But it’s not all smooth sailing. Some people report side effects after switching to a generic - nausea, dizziness, or stomach upset. Why? Because inactive ingredients - fillers, dyes, preservatives - can differ. The FDA allows this. But for people with sensitivities, even a tiny change can matter. In 2023, the FDA received over 1,200 reports of adverse events linked to generic substitutions. Most were gastrointestinal. One common culprit? Lactose. If you’re lactose intolerant, a generic pill with lactose filler can cause real problems. That’s why doctors sometimes stick with brand-name drugs for patients with narrow therapeutic index conditions - like thyroid medication (levothyroxine) or blood thinners (warfarin). Even small differences in absorption can cause harm.
What’s Working - And What’s Not
Let’s compare how different cost-control strategies stack up:| Strategy | Average Savings | Speed of Impact | Scope |
|---|---|---|---|
| Generic substitution | 80-85% | Immediate | Massive - covers 90% of prescriptions |
| Biosimilar adoption | 15-35% | Slow (1-3 years) | Narrow - only 5% of prescriptions |
| Medicare drug price negotiation | 38-79% | Slow (1-2 years) | Very narrow - only 10 drugs in 2026 |
| Step therapy (trying cheaper drugs first) | 12-15% | Variable | Depends on plan |
What Needs to Change
The system works - but it’s being sabotaged by loopholes and incentives that don’t align with patient health. Here’s what needs fixing:- Crack down on pay-for-delay: Make these deals illegal. The FTC has the power - it just needs the will.
- Stop authorized generics: If a brand company wants to make a generic, let them - but don’t let them be the only one. Open the market.
- Fix PBM incentives: PBMs shouldn’t profit more from brand-name drugs. Their fees should be transparent and tied to savings, not list prices.
- Invest in biosimilar development: Offer tax credits, fast-track reviews, and liability shields to encourage companies to enter the biosimilar space.
- Improve prescriber education: Only 37% of doctors can correctly identify when substitution is safe. That’s unacceptable.
Bottom Line: Generics Are the Backbone of Affordable Care
We don’t need to reinvent the wheel. We just need to protect what’s already working. Generics are not a second-tier option. They’re the foundation of affordable healthcare in America. They’re safe. They’re effective. And they’re the single biggest reason prescription drug costs haven’t exploded even faster. The real threat isn’t generics. It’s the forces trying to slow them down - patent games, secret deals, and profit-driven systems that reward high prices over patient access. If we want to control healthcare spending, we don’t need more complex policies. We need to defend and expand the simplest, most proven tool we have: generic drugs.Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence - meaning they deliver the same amount of medicine into the bloodstream at the same rate. Over 90% of generics meet or exceed brand performance in real-world use. Millions of patients take generics every day without issue.
Why do some people say generics don’t work for them?
In rare cases, differences in inactive ingredients - like fillers, dyes, or preservatives - can cause side effects in sensitive individuals. For example, someone with lactose intolerance might react to a generic pill that uses lactose as a filler. This is why doctors sometimes stick with brand-name drugs for narrow therapeutic index medications like levothyroxine or warfarin. But for most people, switching to a generic causes no issues at all.
Why are some generics still expensive?
When only one or two companies make a generic, prices can stay high due to lack of competition. This often happens when manufacturing is complex or the market is small. Sometimes, brand companies delay competition by filing patents or paying generic makers to stay out of the market. These practices are being investigated, but they still happen.
Can pharmacists substitute generics without asking my doctor?
In 48 states, pharmacists can automatically substitute a generic unless the doctor writes “dispense as written” or “no substitution.” Some states require extra steps for high-risk drugs like thyroid meds or seizure medications. Always check your state’s rules - and ask your pharmacist if you’re unsure.
Do generics cause more side effects than brand-name drugs?
No. The FDA reviews all generic drugs for safety and effectiveness before approval. Side effects come from the active ingredient, which is identical in both versions. If you experience new side effects after switching, it’s likely due to inactive ingredients - not the medicine itself. Tell your doctor or pharmacist. They can help you switch to a different generic or go back to the brand.
Are biosimilars the same as generics?
No. Generics are exact copies of simple chemical drugs. Biosimilars are highly similar versions of complex biologic drugs made from living cells. They’re not identical, but they must show no clinically meaningful differences in safety or effectiveness. Biosimilars are harder to make and cost more to develop, so they don’t cut prices as deeply as generics - but they still save billions.
Will Medicare drug price negotiation replace the need for generics?
No. Medicare negotiation only applies to 10 drugs in 2026 - and only for Medicare patients. Generics affect every patient, every day, across all insurance types. Even if Medicare negotiates a 70% discount on a drug, if a generic version is already available, it’s likely already priced lower. Generics are the broadest, fastest, and most reliable way to lower drug costs across the entire system.


Lee M
January 1, 2026 AT 22:12Generics aren't just cheap-they're the ultimate rebellion against corporate greed. The system was built to make you pay for patents, not pills. When you see a $350 insulin bottle and then a $25 generic, you're not seeing a drug-you're seeing the difference between capitalism and survival.
Austin Mac-Anabraba
January 3, 2026 AT 14:31The data is irrefutable: generics reduce spending by 80–85%, yet the pharmaceutical industry still manipulates the market through patent thickets, authorized generics, and pay-for-delay schemes. These are not market failures-they are deliberate, legally sanctioned theft. The Hatch-Waxman Act was a triumph of public policy; what we’re witnessing now is its systematic erosion by rent-seekers who prioritize profit over physiology.
Phoebe McKenzie
January 4, 2026 AT 15:20How is this even legal?! People are CHOOSING between insulin and groceries, and the FDA just shrugs?!! And don’t even get me started on those sneaky pharma companies slapping their own ‘generic’ label on the same damn pill and charging $25 instead of letting real competitors in. This isn’t healthcare-it’s a hostage situation, and we’re all paying ransom!
gerard najera
January 6, 2026 AT 04:16Generics work. The science is settled. The savings are real. The resistance is corporate.
Stephen Gikuma
January 7, 2026 AT 17:3890% generics? That’s not freedom-that’s foreign control. 80% of active ingredients come from China and India. What happens when they cut off supply? We’re not just dependent on pills-we’re dependent on regimes that hate us. This isn’t healthcare policy, it’s national security failure. We need American-made generics, or we’re one war away from mass death.
Layla Anna
January 9, 2026 AT 05:09i just switched my anxiety med to generic and honestly? no difference at all 😊 but my wallet is so happy!! i know some people have issues with fillers but for most of us it’s just the same pill with a cheaper label. thanks for sharing this!! ❤️
Heather Josey
January 9, 2026 AT 18:07It’s remarkable how effective and underappreciated the generic drug system is. We have a tool that saves billions annually, yet we continue to debate complex, slow-moving reforms when the simplest solution is already working. Protecting and expanding access to generics isn’t partisan-it’s practical. We should be celebrating this model, not undermining it with bureaucratic inertia and profit-driven loopholes.
Donna Peplinskie
January 10, 2026 AT 15:38Thank you for writing this so clearly-it’s easy to feel overwhelmed by drug pricing, but seeing the numbers laid out like this gives me hope. I’ve seen friends skip doses because they couldn’t afford brand names, and I’ve seen others panic when their pharmacy switched to a generic. Education matters. So does compassion. Let’s keep pushing for transparency, for access, and for trust in the science behind these life-saving medications.
Olukayode Oguntulu
January 12, 2026 AT 02:57Let’s not romanticize the FDA’s role here. The bioequivalence standard is a statistical mirage-mean AUC and Cmax thresholds are arbitrary thresholds masquerading as scientific rigor. Real-world pharmacokinetic variance is ignored. The FDA approves generics based on group averages, yet individual patients are left to gamble with their neurochemistry. This isn’t healthcare-it’s population-level utilitarianism dressed in lab coats.
jaspreet sandhu
January 13, 2026 AT 08:01People keep saying generics are safe but what about the ones who get sick after switching? I know a guy who took levothyroxine for 10 years and then his pharmacy switched him to generic and he started having heart palpitations and weight gain and his doctor said it was all in his head but he knew better. The body is not a lab rat and the FDA doesn't care about individual biology. They care about averages and profits. And now they want to push biosimilars which are even less understood. This whole system is built on ignoring the small details that matter to real people. You think you're saving money but you're just trading one kind of suffering for another.