Mental Health Screening Calculator
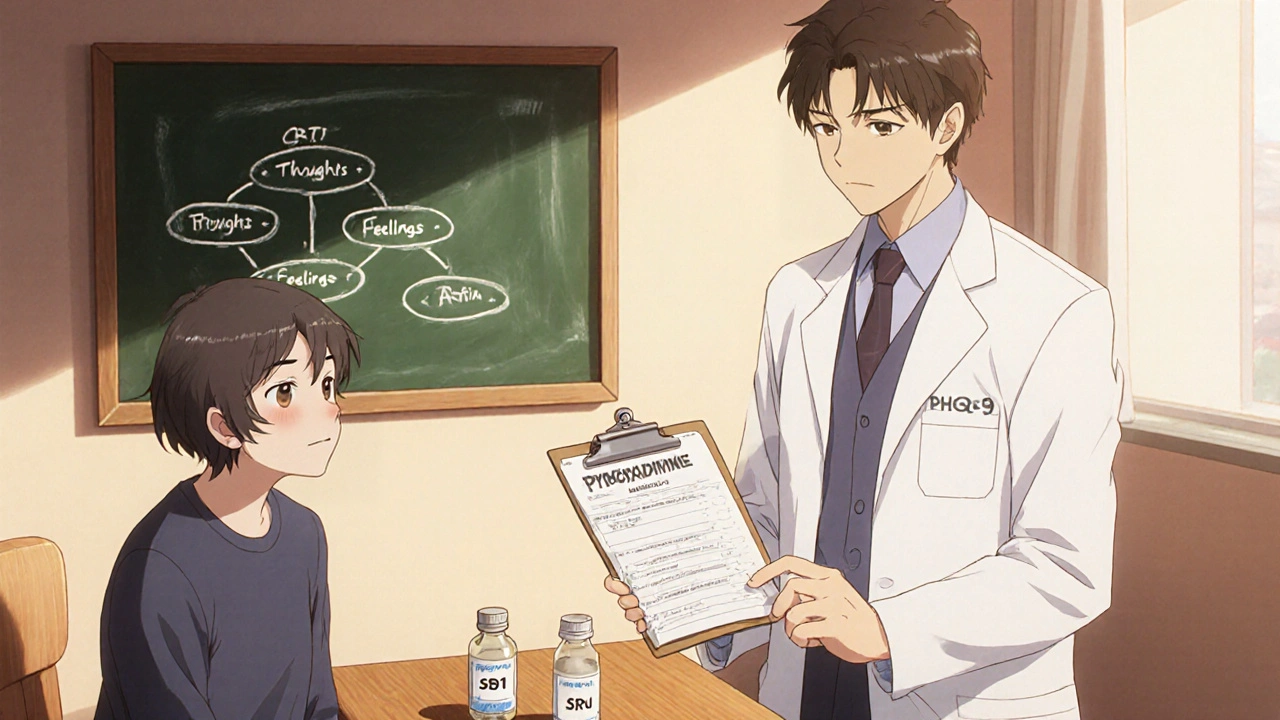
PHQ-9 Depression Screening
Rate how often you've experienced these symptoms in the past 2 weeks:
GAD-7 Anxiety Screening
Rate how often you've experienced these symptoms in the past 2 weeks:
Screening Results
PHQ-9 Score: 0
GAD-7 Score: 0
Quick takeaways
- Ethionamide can trigger depression, anxiety, and even rare psychosis during TB therapy.
- Screening for mood changes at the start of treatment improves outcomes.
- Vitamin B6 (pyridoxine) and short‑acting antidepressants are first‑line mitigations.
- Combining psychosocial support, like CBT, with medical management cuts dropout rates.
- Clinicians should report severe neuropsychiatric events to national pharmacovigilance programs.
When treating multidrug‑resistant tuberculosis, Ethionamide is a second‑line oral antibiotic that works by blocking mycolic acid synthesis in Tuberculosis bacteria. While it saves lives, many patients notice a shift in mood that can feel as unsettling as the disease itself. This article walks through why the drug messes with the brain, how to spot trouble early, and what practical steps patients and providers can take to keep mental health in check.
Why Ethionamide Affects the Brain
Ethionamide belongs to the thioamide class, a chemical family known to cross the blood‑brain barrier. Once inside the central nervous system, it interferes with the synthesis of certain neurotransmitters-especially serotonin and dopamine. Low serotonin levels are a classic recipe for depression, while dopamine disruption can spark anxiety or even transient psychosis.
Research from the World Health Organization (WHO) shows that up to 15 % of MDR‑TB patients on ethionamide report moderate‑to‑severe depressive symptoms, a number that climbs higher when the drug is combined with other neurotoxic agents like cycloserine.
Typical Psychological Side‑Effects
Patients most often describe three categories of symptoms:
- Depression: Persistent sadness, loss of interest, fatigue, and thoughts of hopelessness.
- Anxiety: Restlessness, racing thoughts, and somatic complaints such as a pounding heart.
- Rare psychosis: Hallucinations or delusional thinking, usually appearing after 4‑6 weeks of continuous dosing.
Because these signs overlap with the emotional toll of a TB diagnosis itself, clinicians often miss the drug’s contribution. That’s why systematic screening is critical.
Screening Tools You Can Use Today
Implementing a simple, validated questionnaire at baseline and then every two weeks helps catch mood swings early. The most practical tools are:
- PHQ‑9 for depression - a nine‑item survey that scores each symptom from 0 to 3.
- GAD‑7 for anxiety - seven questions with the same 0‑3 scoring.
- Brief psychosis screen - ask directly about hearing voices or seeing things that aren’t there.
Scores above 10 on PHQ‑9 or GAD‑7 warrant a referral to mental‑health services, even if the patient says they feel “just a little down.”
Medical Strategies to Reduce Neuro‑Psychiatric Risk
Since ethionamide’s chemistry can’t be altered, clinicians rely on adjuncts to balance the brain chemistry:
- Pyridoxine (Vitamin B6): Dosed at 25‑50 mg daily, B6 mitigates peripheral neuropathy and may blunt some neurotoxic effects.
- Selective serotonin reuptake inhibitors (SSRIs): Fluoxetine 20 mg daily has shown rapid improvement in ethionamide‑related depression without compromising TB drug levels.
- Low‑dose antipsychotics: Risperidone 0.5‑1 mg can be introduced if psychotic symptoms emerge, tapering off once the drug is discontinued.
All medication adjustments should be coordinated with the TB treatment team to avoid drug‑drug interactions-especially with rifampicin, which can lower SSRI concentrations.
Psychosocial Interventions That Make a Difference
Medication alone rarely solves the problem. Studies from South Africa’s MDR‑TB clinics demonstrate that adding Cognitive Behavioral Therapy (CBT) to the standard directly observed treatment, short‑course (DOTS) program improves adherence by 30 %.
Key CBT techniques for TB patients include:
- Reframing catastrophic thoughts about the disease.
- Behavioral activation-scheduling small, rewarding activities each day.
- Relaxation training to lower physiological anxiety.
Group counseling also helps; hearing peers share coping tactics reduces isolation, a known driver of depression.
Comparing Neuro‑Psychiatric Profiles of Common TB Drugs
| Drug | Depression Risk | Anxiety/Insomnia | Psychosis | Management Tips |
|---|---|---|---|---|
| Ethionamide | Medium‑High | Medium | Low‑Medium (rare) | Pyridoxine, SSRIs, close monitoring |
| Isoniazid | Medium (linked to B6 deficiency) | High (insomnia common) | Very Rare | Pyridoxine supplementation |
| Rifampicin | Low | Low | Very Rare | Screen for drug interactions |
| Cycloserine | High | High | Medium (psychosis reported) | SSRIs, dose titration, mental‑health referral |
The table shows that ethionamide sits in the middle of the risk spectrum-higher than rifampicin but lower than cycloserine. Knowing where the drug lands helps clinicians decide how aggressively to screen.
Case Study: Turning a Mood Crisis into a Success Story
Maria, a 34‑year‑old teacher from New Delhi, began an MDR‑TB regimen that included ethionamide, cycloserine, and levofloxacin. Six weeks in, she reported nightly insomnia and persistent low mood. Her PHQ‑9 score hit 14, flagging moderate depression.
The clinic added pyridoxine 50 mg and started fluoxetine 20 mg. Simultaneously, a social worker enrolled her in a weekly CBT group. Within a month, Maria’s PHQ‑9 dropped to 6, and she completed treatment without missing a single DOTS dose.
This example underscores how a combined medical‑psychosocial plan can prevent treatment abandonment-a major cause of TB resistance.
Reporting and Pharmacovigilance
Whenever severe neuro‑psychiatric events occur, they should be logged in the national pharmacovigilance system. In the United States, the FDA’s MedWatch program captures such data, which later informs label updates.
Key reporting elements include:
- Exact drug dose and duration.
- Onset timing of symptoms.
- Any concurrent medications (especially other neuroactive agents).
- Outcome after intervention (recovery, continuation, or discontinuation).
Systematic reporting not only protects the individual patient but also builds a safety database that benefits future TB cohorts.
Practical Checklist for Clinicians and Caregivers
- Baseline mental‑health screen (PHQ‑9, GAD‑7).
- Prescribe pyridoxine 25‑50 mg daily from day 1.
- Schedule follow‑up mental‑health assessment every 2 weeks.
- Have a low‑threshold plan for SSRIs or antipsychotics if scores rise.
- Enroll patient in CBT or peer‑support groups where available.
- Document any neuro‑psychiatric events and report through MedWatch or local equivalents.
Running through this list each month helps keep the invisible side‑effects visible and manageable.
Looking Ahead: Research Gaps and Future Directions
Despite growing awareness, many questions linger:
- Would a lower ethionamide dose retain efficacy while reducing mood impact?
- Can genetic testing predict who’s most vulnerable to neuro‑psychiatric toxicity?
- How do digital mental‑health interventions (e.g., mobile CBT apps) perform in low‑resource TB settings?
Answering these will require collaboration between TB programs, psychiatry researchers, and pharmacogenomics labs.
What is the most common mental‑health side effect of ethionamide?
Depression tops the list, affecting roughly 10‑15 % of patients on standard MDR‑TB regimens that include ethionamide.
Should every patient on ethionamide receive an antidepressant automatically?
No. Antidepressants are added after a screening score indicates moderate‑to‑severe symptoms, or if the patient has a prior mood‑disorder history.
How long do mood changes usually last after stopping ethionamide?
Most patients see improvement within 2‑4 weeks of drug cessation, especially if supportive therapy is continued.
Can pyridoxine prevent depression caused by ethionamide?
Pyridoxine mainly thwarts peripheral neuropathy, but it also appears to modestly lower depression scores, likely by supporting neurotransmitter synthesis.
Is it safe to combine fluoxetine with rifampicin?
Rifampicin can accelerate fluoxetine metabolism, reducing its blood level. If needed, clinicians often increase fluoxetine to 40 mg or choose an antidepressant less affected by liver enzymes.


Angela Koulouris
October 21, 2025 AT 14:49Hang in there; a little Vitamin B6 can brighten the mood like a sunrise.
Harry Bhullar
November 2, 2025 AT 03:36Ethionamide’s ability to cross the blood‑brain barrier means it can meddle with neurotransmitter synthesis, which is why mood swings pop up for many patients.
The first thing to do is a baseline PHQ‑9 and GAD‑7 before the drug even starts, so you have a reference point.
Then schedule a follow‑up every two weeks; the data show that early detection cuts dropout rates dramatically.
If the PHQ‑9 climbs above ten, consider adding pyridoxine at 25‑50 mg daily, because it can cushion peripheral neurotoxicity and may ease depressive symptoms.
At the same time, a low‑dose SSRI such as fluoxetine 20 mg can be started, but remember rifampicin may accelerate its metabolism, so monitor levels or bump the dose to 40 mg if needed.
For anxiety, a short course of an anxiolytic like buspirone can calm the racing heart while you wait for the SSRI to kick in.
In cases where psychotic features appear, a low‑dose antipsychotic like risperidone 0.5 mg is a reasonable bridge until ethionamide is stopped.
Don’t forget non‑pharmacologic tools: CBT groups have been shown to lift adherence by about thirty percent in MDR‑TB clinics.
Teaching patients to schedule pleasant activities each day, even something as simple as a walk, can counteract the “flat” feeling that often accompanies depression.
Peer support, whether in person or via a WhatsApp group, also reduces the isolation that fuels both anxiety and hopelessness.
All of these interventions should be coordinated with the TB treatment team to avoid drug‑drug interactions, especially with rifampicin’s enzyme‑inducing effects.
Document any neuro‑psychiatric event in the national pharmacovigilance system; the more data we have, the better future guidelines will be.
Genetic testing is still experimental, but early studies suggest certain CYP polymorphisms might predict who’s most vulnerable to ethionamide’s brain effects.
In low‑resource settings, even a paper‑based checklist covering the six bullet points in the article can make a huge difference.
Bottom line: proactive screening, prompt adjunct therapy, and psychosocial support together turn a potentially destabilizing side effect into a manageable part of the TB cure journey.
Dana Yonce
November 13, 2025 AT 17:23Those mood checks are super helpful 😊. Even a quick “how are you feeling?” can catch a dip before it spirals.
Lolita Gaela
November 25, 2025 AT 07:09To expand on the pharmacokinetic nuance you mentioned, ethionamide is metabolized via hepatic N‑acetyltransferase pathways, and co‑administration with rifampicin can induce CYP3A4, reducing plasma concentrations of concomitant SSRIs. This bidirectional interaction necessitates therapeutic drug monitoring (TDM) when fluoxetine or sertraline are employed. Moreover, the inhibition of pyridoxal‑5′‑phosphate-dependent enzymes contributes to the observed neuropsychiatric phenotype, which aligns with the reported elevation in homocysteine levels. Clinicians should thus consider serial homocysteine assays alongside PHQ‑9 scoring to delineate etiologic contributions. Lastly, integrating a structured CBT protocol, such as the Beck Youth Inventories adapted for adult TB cohorts, standardizes the psychosocial component across multidisciplinary teams.
Giusto Madison
December 6, 2025 AT 20:56Look, if you’re still thinking the mood shifts are “just part of TB,” you’re ignoring hard data-ethionamide consistently ranks in the medium‑high depression risk column. You need a baseline screen, period, and if scores jump, hit the SSRI fast; waiting is a luxury patients can’t afford.
Ashok Kumar
December 18, 2025 AT 10:43Yeah, because who has time to “wait” when you’re already juggling a 20‑month drug regimen, right? A little sarcasm aside, a quick pill of pyridoxine and a brief counseling session can actually save weeks of misery.
Sakib Shaikh
December 30, 2025 AT 00:29Yo, everyone actully overhypes the “depression” thing – it’s just a lil' mood swing, not a full‑blown crisis. Get over it, take the med, and stop blowing it up.
Devendra Tripathi
January 10, 2026 AT 14:16Hold up, dismissing documented neuro‑psychiatric side effects as “just a mood swing” is reckless. The WHO data you ignore shows up to 15 % of patients suffer moderate‑to‑severe depression, and that’s a public‑health concern, not a meme.
Vivian Annastasia
January 22, 2026 AT 04:03Wow, look who’s finally done their homework. Maybe next time you’ll cite the exact article instead of echoing a headline. But hey, thanks for the reminder that we need “serious” data before we panic.