Medication Safety Symptom Checker
Check Your Symptoms
Enter symptoms you're experiencing since starting a new medication. This tool identifies potentially dangerous reactions based on FDA guidelines.
Taking medication should help you feel better-not put you in danger. But sometimes, a drug that’s meant to treat one problem can trigger another, more serious one. The truth is, dangerous medication side effects don’t always come with a warning label you can see coming. Some start as a mild itch. Others begin with a strange dizziness or a sudden nausea. By the time you realize something’s wrong, it might already be too late. The good news? There are clear, early signs that can tell you when to act-before it becomes an emergency.
What Makes a Side Effect Dangerous?
Not all side effects are created equal. A dry mouth, a little drowsiness, or an upset stomach? Those are common. They happen to about 35% of people taking prescription meds, according to the FDA. But dangerous side effects? Those are rare-only about 0.1% of medication courses lead to them. Yet, they cause over 1.3 million emergency room visits every year in the U.S. alone. A side effect becomes dangerous when it threatens your life, causes permanent damage, or requires hospitalization. The FDA defines serious reactions as those that lead to death, life-threatening conditions, organ failure, or birth defects. Think of it this way: if your body is screaming for help, don’t wait to see if it gets quieter. Listen.Red Flags That Need Immediate Action
Some symptoms can’t be ignored. If you notice any of these after taking a new medication-or even an old one you’ve taken before-call 911 or go to the nearest ER right away:- Difficulty breathing or tightness in your throat
- Swelling of your face, lips, tongue, or throat
- Hives or a sudden rash that spreads quickly
- Chest pain or pressure that doesn’t go away
- Heart rate over 120 beats per minute with dizziness or fainting
- Seizures or convulsions
- Black, tarry stools or vomiting blood
- Yellowing of skin or eyes (jaundice) with severe stomach pain
- Extreme confusion, inability to wake up, or unresponsiveness
Signs That Are Slower-but Just as Dangerous
Not all life-threatening reactions happen in minutes. Some creep up over days or weeks. That’s why it’s easy to miss them.- Unusual bruising or bleeding-even from minor bumps. This could mean your blood isn’t clotting right, a side effect of blood thinners, NSAIDs, or even some antibiotics.
- Dark urine or no urine at all. If you’re not peeing like you used to, your kidneys might be struggling. This is especially common with diabetes drugs like semaglutide or certain painkillers.
- Extreme fatigue paired with a rapid heartbeat or shortness of breath. That’s not just "being tired." It could be drug-induced anemia, where your body stops making enough red blood cells.
- Swelling in your legs or belly with weight gain you can’t explain. Fluid retention can signal liver or heart damage from medications like NSAIDs, steroids, or some blood pressure drugs.
- Fever, joint pain, and rash appearing together. This trio could mean DRESS syndrome-a rare but deadly reaction that attacks your skin, liver, and kidneys.

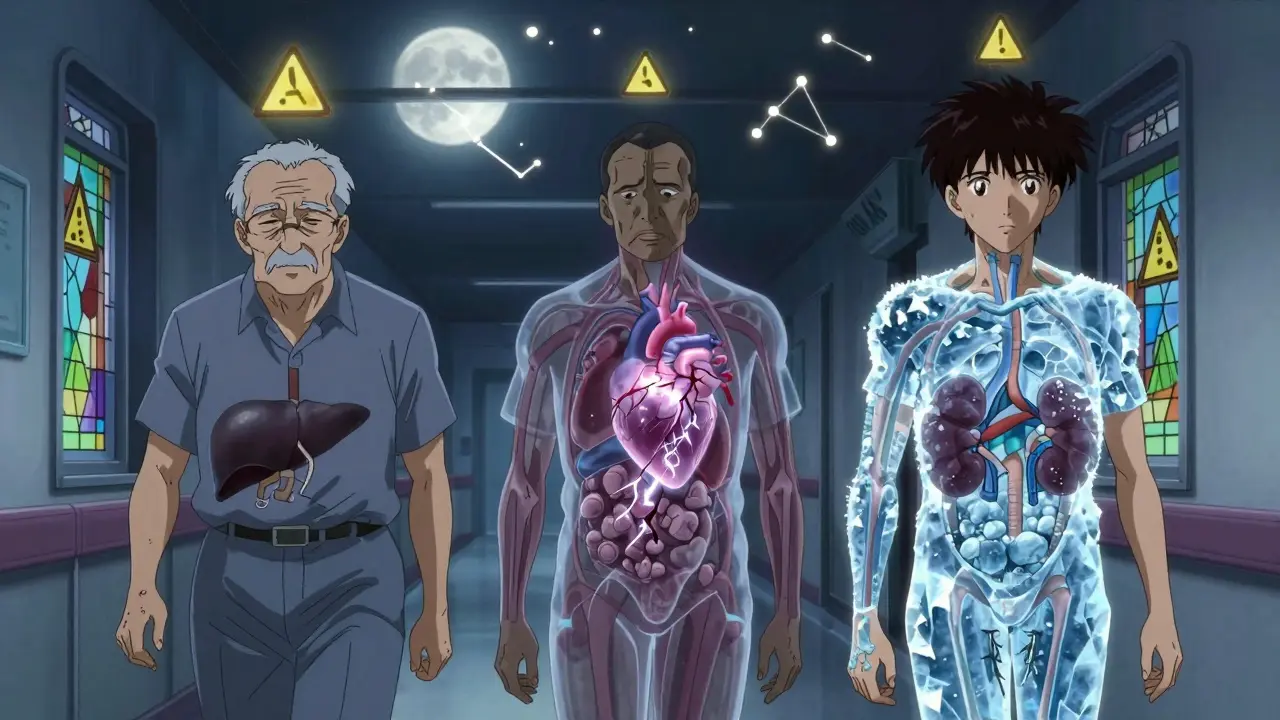
Why Some People Are at Higher Risk
You might think, "It won’t happen to me." But certain factors make dangerous reactions more likely:- Age 65+: Your body processes drugs slower. The American Geriatrics Society says older adults have side effects 2.7 times more often than younger people.
- Taking five or more medications: That’s called polypharmacy. It increases your risk of dangerous interactions by 300%. Insulin and heparin are two of the most commonly confused drugs-mix-ups can be fatal.
- Existing liver or kidney disease: These organs filter out drugs. If they’re already weak, toxins build up faster.
- Genetic factors: New testing can now show if you’re genetically prone to bad reactions. For example, people with a certain gene variant react dangerously to carbamazepine (an epilepsy drug). Testing before prescribing can cut severe reactions by nearly half.
What to Do When You Notice a Problem
Don’t panic. But don’t wait either. Here’s what to do based on the symptom:- Life-threatening signs (breathing trouble, swelling, chest pain, seizure): Call 911 immediately. Don’t drive yourself. Don’t call your doctor first. Emergency responders carry epinephrine and can start treatment on the way.
- Unusual bleeding, jaundice, severe nausea, or confusion: Contact your prescribing provider within 24 hours. If you can’t reach them, go to urgent care. Don’t wait until your next appointment.
- New rash, mild swelling, or fatigue: Note when it started, how it changed, and what meds you took. Bring this info to your next visit. Take a photo of the rash if possible.
- Never stop a prescribed medication cold turkey. Stopping beta-blockers, antidepressants, or seizure meds suddenly can cause seizures, heart attacks, or severe withdrawal. Always talk to your doctor first.
How to Protect Yourself Before It Happens
Prevention beats reaction every time. Here’s how:- Use the Brown Bag Method: Every three months, gather all your meds-pills, vitamins, supplements, OTC drugs-and take them to your doctor or pharmacist. Many dangerous side effects come from hidden interactions.
- Ask about genetic testing: If you’re prescribed a high-risk drug like carbamazepine, warfarin, or abacavir, ask if a simple blood test can predict your risk.
- Know your meds: Read the patient information sheet. Look for words like "serious," "life-threatening," or "seek immediate medical help." If you don’t understand it, ask.
- Track changes: Keep a simple log: date, medication, dose, and any new symptom-even if it seems small. A change in sleep, appetite, or mood can be a clue.
- Use technology: New AI tools are now being used in clinics to predict side effects based on your age, weight, kidney function, and other meds. Ask if your provider uses them.
When to Call Your Doctor-Even If It Feels Minor
You don’t need to wait for a crisis. If you notice any of these, call your provider:- A new rash that doesn’t go away
- Unexplained weight gain or loss
- Increased dizziness or unsteadiness when walking
- Changes in vision or hearing
- Persistent headaches
- Feeling "off" in a way you can’t explain
Medications save lives. But they can also harm them-sometimes quietly. The key isn’t avoiding drugs. It’s knowing what to watch for, acting fast, and staying in charge of your own health. You know your body better than anyone else. Trust your gut. If something feels wrong, it probably is.
Can a medication cause dangerous side effects even if I’ve taken it before without problems?
Yes. Your body changes over time. Liver or kidney function slows with age. New medications can interact with old ones. Even your diet or alcohol use can change how your body processes a drug. A medication that was safe last year might become dangerous this year. That’s why regular medication reviews are so important.
How long after taking a medication do dangerous side effects usually appear?
It varies. Severe allergic reactions like anaphylaxis often happen within minutes to an hour. Rashes or liver problems can take days or weeks. Some reactions, like DRESS syndrome, may not show up until 2-6 weeks after starting the drug. If you notice a new symptom after starting a medication-even weeks later-it’s worth checking out.
Are over-the-counter drugs and supplements safer than prescription meds?
No. Many people assume OTC meds are harmless, but that’s dangerous. NSAIDs like ibuprofen can cause internal bleeding. Herbal supplements like St. John’s Wort can interfere with antidepressants and birth control. Even common vitamins like vitamin E or fish oil can thin your blood. About 20% of serious drug reactions involve OTC drugs or supplements.
What should I do if I can’t reach my doctor when I notice a problem?
If it’s life-threatening, call 911. If it’s serious but not emergency-level (like new jaundice or unusual bleeding), go to an urgent care center or ER. They can evaluate you, stabilize you, and contact your doctor. Never wait for a callback if you feel something’s seriously wrong.
Is it safe to stop a medication if I think it’s causing side effects?
Only if your doctor tells you to. Stopping certain drugs suddenly-like beta-blockers, antidepressants, or seizure meds-can cause rebound effects that are more dangerous than the original side effect. Always talk to your provider first. They may recommend tapering off slowly or switching to another drug.

Niel Amstrong Stein
February 7, 2026 AT 20:09Mary Carroll Allen
February 8, 2026 AT 10:15Sarah B
February 8, 2026 AT 21:56Paula Sa
February 9, 2026 AT 17:42Amit Jain
February 11, 2026 AT 05:14AMIT JINDAL
February 11, 2026 AT 09:04Savannah Edwards
February 13, 2026 AT 03:42Tola Adedipe
February 14, 2026 AT 01:25Ritu Singh
February 14, 2026 AT 10:47Mark Harris
February 15, 2026 AT 19:25Marcus Jackson
February 16, 2026 AT 05:20Natasha Bhala
February 18, 2026 AT 03:41Joey Gianvincenzi
February 18, 2026 AT 11:51Eric Knobelspiesse
February 19, 2026 AT 18:50Gouris Patnaik
February 20, 2026 AT 17:32