When you’re pregnant and struggling with severe anxiety or insomnia, the pressure to find relief is real. Many women turn to benzodiazepines-medications like lorazepam, alprazolam, or diazepam-because they work quickly and effectively. But what happens when you’re carrying a baby? The answer isn’t simple. While these drugs help manage symptoms, growing evidence suggests they might also raise the risk of serious birth defects. This isn’t scare tactics. It’s science. And if you’re pregnant or planning to be, you need to know what the data actually says.
What Are Benzodiazepines, and Why Are They Used in Pregnancy?
Benzodiazepines are a class of drugs first developed in the 1950s. They calm the nervous system, reduce anxiety, help with sleep, and can prevent seizures. For some women, these effects are lifesaving. About 1.7% of pregnant women in the U.S. get a prescription for one during the first trimester, and that number has been rising. Why? Because anxiety and insomnia affect roughly 1 in 6 women of childbearing age. When therapy or lifestyle changes don’t cut it, doctors sometimes reach for a benzodiazepine.
But here’s the catch: these drugs cross the placenta. That means whatever you take, your baby takes too. And because fetal organs are forming in the first trimester, that’s when exposure is most risky. The developing brain, heart, and facial structures are especially sensitive to chemical disruptions.
What Birth Defects Are Linked to Benzodiazepines?
Not all birth defects are equally likely. The biggest red flags come from large studies tracking hundreds of thousands of pregnancies.
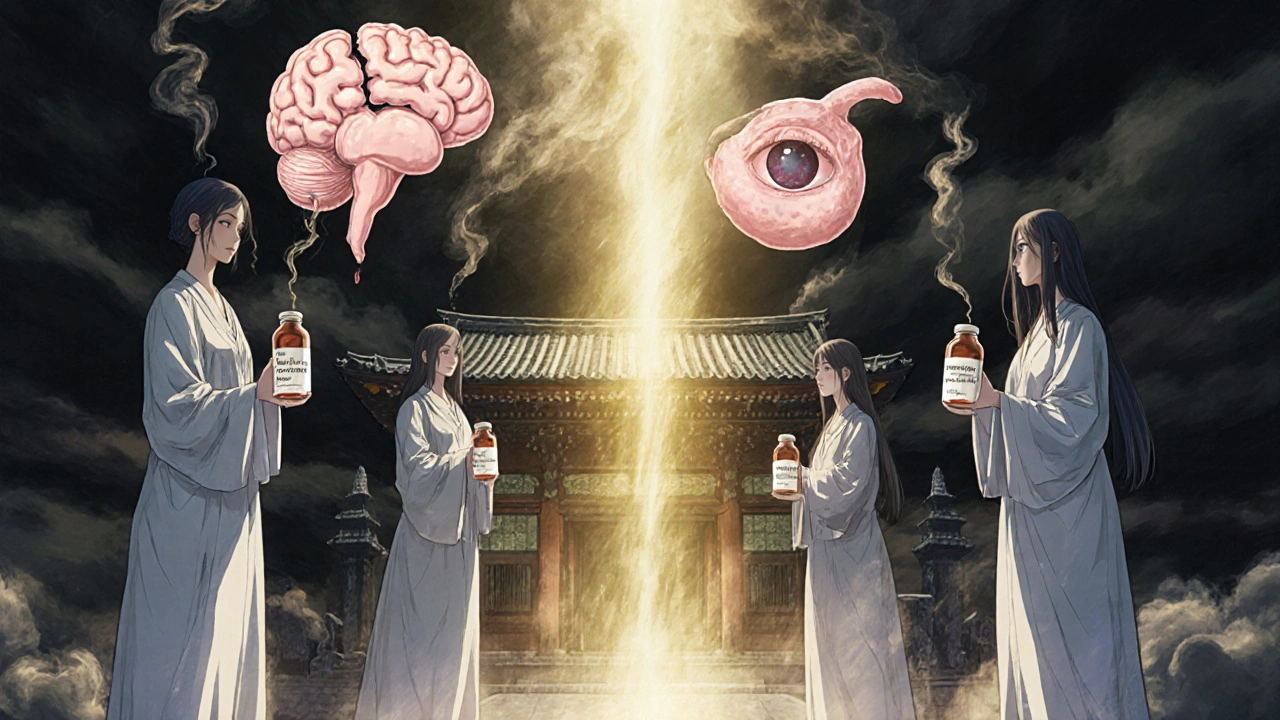
- Dandy-Walker malformation: A rare but serious brain defect where part of the cerebellum doesn’t form properly. One study found a threefold increase in risk with benzodiazepine exposure.
- Anophthalmia or microphthalmia: Missing or underdeveloped eyes. This was strongly linked to alprazolam-the brand-name drug Xanax. The risk was four times higher in women who took it during early pregnancy.
- Esophageal atresia: A condition where the esophagus doesn’t connect properly to the stomach. Again, alprazolam was the main driver of this risk.
- Heart defects: Particularly structural problems like pulmonary valve stenosis. Lorazepam (Ativan) showed a clear association here.
These aren’t common. But they’re severe. For every 1,000 women taking benzodiazepines in the first trimester, about 8 more babies will have a major birth defect compared to those who don’t. For heart defects, that number jumps to 14 extra cases per 1,000 pregnancies.
It’s not all benzodiazepines, either. Alprazolam stands out in multiple studies as the highest-risk agent. Diazepam and lorazepam show more mixed results, but still carry risk. Clonazepam? Data is limited, but caution is still advised.
What About Other Pregnancy Risks?
Birth defects aren’t the only concern. Benzodiazepines are tied to a range of other complications:
- Miscarriage: Risk increases by about 85% when taken during pregnancy.
- Preterm birth: Babies born before 37 weeks are more common in exposed pregnancies.
- Low birth weight: Babies tend to weigh less, even when born at full term.
- Neonatal withdrawal: Babies born to mothers who took benzodiazepines late in pregnancy can have jitteriness, poor feeding, breathing problems, or seizures in the first days after birth.
- Ectopic pregnancy: Even taking these drugs in the 90 days before conception raises the risk.
These outcomes aren’t just statistics. They mean longer hospital stays, NICU admissions, and sometimes lifelong care needs.
Why Do Some Studies Say There’s No Risk?
You might have seen headlines claiming benzodiazepines are safe in pregnancy. That’s because not all studies agree. One 2023 study from the British Journal of Clinical Pharmacology found no link to birth defects. So which one do you believe?
The difference lies in study design. Many early studies didn’t account for confounding by indication. That means: women taking benzodiazepines often have severe anxiety, depression, or other mental health conditions-and those conditions themselves can increase pregnancy risks. So is it the drug, or the illness behind it?
The most reliable studies, like the 2022 PLOS Medicine analysis of 3.1 million pregnancies, used advanced methods to separate drug effects from underlying illness. They even ran negative control tests-looking at outcomes that shouldn’t be affected by the drug-and found no false signals. That strengthens the case that the risks are real.
Plus, the PLOS Medicine study had over 10 times more exposed pregnancies than all previous studies combined. That kind of power matters.
What Do Medical Guidelines Say?
Major medical groups are clear: avoid benzodiazepines in pregnancy if you can.
- ACOG (American College of Obstetricians and Gynecologists): Says benzodiazepines “may be used cautiously for short-term treatment,” but should be avoided in the first trimester.
- American Psychiatric Association: Recommends case-by-case decisions, with special attention to the drug, dose, and timing.
- Canadian Clinical Practice Guidelines: States benzodiazepines “should generally be avoided during pregnancy,” especially in the first trimester.
- FDA: Classifies all benzodiazepines as Category D-meaning there’s proven risk to the fetus.
- European Medicines Agency: Recommends avoiding them in the first trimester unless absolutely necessary.
There’s no blanket “safe” option. But the consensus is strong: if you don’t need it, don’t take it.

What Are the Alternatives?
If you’re pregnant and anxious or struggling to sleep, you’re not out of options.
- Cognitive Behavioral Therapy (CBT): Proven to work as well as medication for anxiety and insomnia during pregnancy. No side effects. No risk to the baby.
- Mindfulness and meditation: Studies show these reduce cortisol levels and improve sleep quality.
- Exercise: Even 30 minutes of walking a day lowers anxiety and improves mood.
- Support groups: Talking to other pregnant women with similar struggles reduces isolation and stress.
- SSRIs (like sertraline): If you need medication, some antidepressants are better studied and carry lower risks than benzodiazepines. Sertraline is often the first choice.
And yes-these alternatives take time. They’re not a quick fix. But they’re safer. And they build skills you’ll use long after your baby is born.
What Should You Do If You’re Already Taking Benzodiazepines?
If you’re pregnant and currently on a benzodiazepine, do not stop cold turkey. Sudden withdrawal can trigger seizures, extreme anxiety, or even harm your baby.
Instead:
- Call your OB-GYN or psychiatrist right away.
- Don’t change your dose without professional guidance.
- Ask about tapering off slowly-over weeks or months, depending on your dose and how long you’ve been taking it.
- Start non-drug therapies now. Even small steps help.
- Keep track of your symptoms. Write down when you feel anxious or can’t sleep. That helps your provider adjust your plan.
Some women need to stay on medication. If your anxiety is so severe it stops you from eating, sleeping, or caring for yourself, the risks of untreated illness may outweigh the risks of the drug. That’s a decision you make with your doctor-not alone, not on the internet.
Bottom Line: Weighing Risk and Reality
Let’s be honest: no medication is 100% safe in pregnancy. But benzodiazepines are among the highest-risk classes. The data is clearer now than ever. For most women, the benefits don’t outweigh the potential harm.
That doesn’t mean you’re failing if you’ve taken them. It doesn’t mean you’re a bad mom. It just means you need better tools.
The goal isn’t perfection. It’s safety. And safety means choosing options with the least risk to your baby-while still taking care of your mental health.
If you’re pregnant and anxious, you’re not alone. And you don’t have to suffer-or risk your baby’s health-to find relief. There are safer paths. You just need the right support to find them.
Can I take benzodiazepines while breastfeeding?
Some benzodiazepines pass into breast milk, and while the amounts are usually small, they can make your baby sleepy, weak, or have trouble feeding. Short-acting drugs like lorazepam are preferred if absolutely necessary, but even then, use the lowest dose for the shortest time. Avoid alprazolam-it builds up in breast milk and can cause more sedation in the baby. Always talk to your doctor before using any medication while nursing.
Is it safe to take benzodiazepines in the second or third trimester?
The biggest risk for birth defects is in the first trimester, when organs are forming. But taking benzodiazepines later in pregnancy still carries risks: preterm birth, low birth weight, and neonatal withdrawal. Babies exposed in the third trimester may need monitoring after birth for breathing problems, irritability, or feeding difficulties. If you need medication later in pregnancy, your doctor may consider alternatives with better safety profiles.
Which benzodiazepine is safest during pregnancy?
No benzodiazepine is truly safe during pregnancy. But if one must be used, lorazepam (Ativan) is often preferred because it’s metabolized quickly and doesn’t build up as much in the body. Diazepam (Valium) stays in the system longer and is linked to more complications. Alprazolam (Xanax) carries the highest risk for specific birth defects like eye and esophageal malformations. The best approach is to avoid all of them if possible.
What should I do if I took benzodiazepines before I knew I was pregnant?
Don’t panic. Many women take these medications before realizing they’re pregnant. The absolute risk of a major birth defect is still low-even with exposure. Talk to your provider about your specific drug, dose, and timing. They may recommend a detailed anatomy ultrasound around 18-22 weeks to check for structural issues. Most babies exposed to benzodiazepines early on are born healthy. The key is to stop taking them now and move to safer options.
Are there any long-term effects on children exposed to benzodiazepines in utero?
Research is still emerging, but some studies suggest possible links to subtle developmental delays, attention problems, or behavioral issues later in childhood. These effects are not guaranteed and are often small, but they add another layer to the risk-benefit analysis. Long-term monitoring is recommended for children exposed during pregnancy, especially if they had neonatal withdrawal symptoms.


Jim Oliver
November 8, 2025 AT 02:15Let’s be real-anyone who takes Xanax while pregnant deserves whatever happens. It’s not rocket science. You want to numb your feelings? Fine. But don’t blame the baby when it’s born with no eyes. That’s not bad luck-that’s bad choices.
William Priest
November 9, 2025 AT 00:27bro i took ativan for 3 months when i was preggo and my kid is now 7 and runs faster than the wind. also he reads at a 12th grade level. so uh... maybe the study is wrong? or maybe im just a miracle worker?
Ryan Masuga
November 10, 2025 AT 16:47Hey-I get it. Anxiety doesn’t care if you’re pregnant. But you’re not alone. I was on benzos too. Switched to CBT, started yoga, and honestly? I feel better than ever. No meds. No guilt. Just me, my baby, and a whole lot of deep breaths. You got this.
Jennifer Bedrosian
November 11, 2025 AT 17:11ok so i took xanax when i didnt even know i was pregnant and now my daughter is 2 and she’s literally a genius and also a tiny ninja who climbs curtains. so maybe its not that bad? also i cried for 3 hours after reading this article so thank you for that
Lashonda Rene
November 12, 2025 AT 15:58i just want to say that i think this is really important but also i think people shouldnt be shamed for taking medicine when they need it because mental health is health and if you are so overwhelmed that you cant even get out of bed then maybe the risk of the medicine is less than the risk of not taking it and also i think doctors should be more honest about how hard it is to find alternatives because cbt is great but its not always available and sometimes its six months waitlist and by then you might be 20 weeks along and already scared to death so maybe we need more support not more judgment
Andy Slack
November 14, 2025 AT 05:59Knowledge is power. This post saved me from a bad decision. I was about to refill my alprazolam script. Now I’m calling my therapist. Thanks for laying it out like this. No fluff. Just facts. That’s what we need.
Rashmi Mohapatra
November 15, 2025 AT 12:59you americans always overreact. in india we give diazepam to pregnant women since 1970s. no one cares. babies are fine. you just need to trust god and stop watching scary internet articles
Abigail Chrisma
November 15, 2025 AT 16:44For anyone reading this who’s scared or ashamed-please know your worth isn’t measured by your medication choices. You’re not failing. You’re surviving. And now you’re learning. That’s courage. Reach out. Talk to someone. You don’t have to do this alone.
Ankit Yadav
November 15, 2025 AT 19:44the data is strong but i think we need to talk about access too. cbt is great but what if you live in a rural area with no therapists? what if you have no insurance? what if your job doesn’t give you time off? the system fails people before they even get to the pill bottle
Meghan Rose
November 17, 2025 AT 07:52Wait, so if I took lorazepam at 6 weeks and now I’m 14 weeks… am I going to have a baby with no esophagus? Should I just abort? Did you even consider that maybe some of us didn’t know we were pregnant? Do you think we’re monsters? I’m crying right now and you’re just listing statistics like a robot.
Steve Phillips
November 19, 2025 AT 05:03Oh, here we go-the ‘science says’ parade. Again. Let’s not forget the 2023 British study that said NO RISK. But sure, let’s ignore that one because it didn’t fit the narrative. This isn’t science-it’s fearmongering dressed up as public health. And now we’re making women feel guilty for being human.
Rachel Puno
November 20, 2025 AT 07:45Hey-I was in your shoes. Took benzos for insomnia. Then found out I was pregnant. Panic. Then I found a doula who specialized in mental health. We started light walking, journaling, and breathing exercises. Within two weeks, my anxiety dropped. No meds. No guilt. Just me and my growing bump. You can do this too.
Clyde Verdin Jr
November 21, 2025 AT 17:45So… you’re saying if I took Xanax and my kid has a cleft palate… it’s my fault? What if I had no access to therapy? What if my doctor prescribed it? What if I was suicidal? Oh wait-nope, we’re just supposed to ‘suck it up’ and meditate. Yeah right. This post is just another way to punish women who are already drowning.
Key Davis
November 22, 2025 AT 13:30While the epidemiological data presents a compelling case for caution, it is imperative that clinical decisions remain individualized and grounded in patient-centered care. The ethical obligation to mitigate fetal risk must be balanced with the imperative to preserve maternal psychological integrity. A rigid, one-size-fits-all approach risks exacerbating harm through untreated psychiatric illness.
Cris Ceceris
November 22, 2025 AT 22:23I wonder… if we stopped treating anxiety like a flaw to be fixed with chemicals, and started treating it like a signal that something in a person’s life needs support-would we be having this conversation at all? Maybe the real problem isn’t the drug. Maybe it’s the world that makes people feel like they need to numb themselves just to survive.