Every year, thousands of seniors are told to stop their blood thinners because they fell once - maybe even just tripped over a rug. But here’s the truth most doctors don’t say out loud: anticoagulants save more lives than they endanger in older adults with atrial fibrillation. The fear of falling is real. The risk of stroke? It’s worse.
Why Seniors Need Blood Thinners
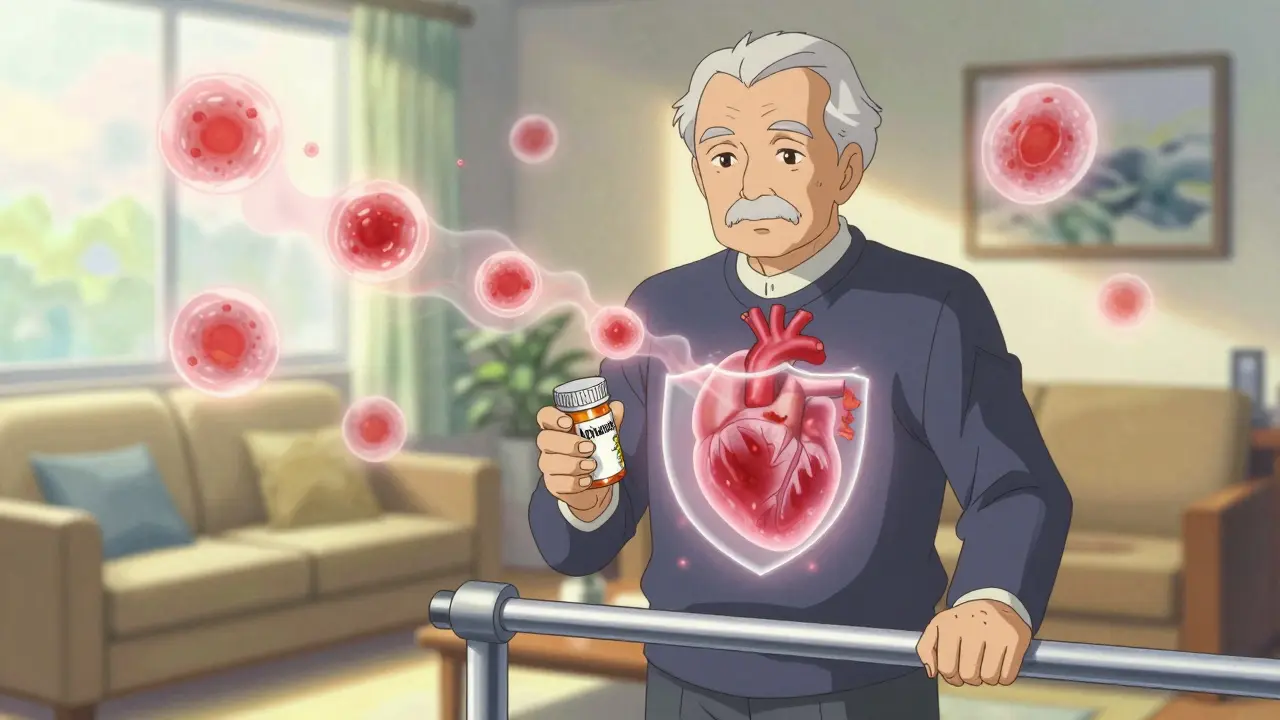
Atrial fibrillation - or AFib - is an irregular heartbeat that affects about 9% of people over 65. It doesn’t just cause fluttering or fatigue. It lets blood pool in the heart, where clots can form. Those clots can travel to the brain and cause a stroke. The older you are, the higher the risk. At age 70-79, your chance of having a stroke from AFib jumps to nearly 10% per year. By 80-89, it’s over 23%. That’s more than one in four people.Without treatment, AFib turns into a ticking time bomb. But anticoagulants - commonly called blood thinners - cut that risk in half or even more. Warfarin, used since the 1950s, reduces stroke risk by about 64%. Newer drugs like apixaban, rivaroxaban, and dabigatran do just as well, sometimes better. And they don’t need weekly blood tests like warfarin does.
The Fall Fear: Real, But Overblown
It’s easy to see why families panic. A senior falls. A head injury follows. A bleed in the brain happens. It’s tragic. And yes - people on anticoagulants who fall are more likely to have serious bleeding. Minnesota hospital data shows they have a 50% higher chance of intracranial hemorrhage than those not on blood thinners.But here’s what most people miss: most strokes kill faster than falls. A stroke can leave someone paralyzed, unable to speak, or dead within minutes. A fall might mean a broken hip - painful, yes, but often treatable. Studies tracking thousands of seniors over decades show that the chance of having a stroke from untreated AFib is far greater than the chance of dying from a fall while on anticoagulants.
The BAFTA trial, which studied 248 patients with an average age of 81.5, found that those on anticoagulants had 52% fewer strokes than those on aspirin. And there was no significant increase in major bleeding. The same pattern showed up in ARISTOTLE and RE-LY trials - even in people over 90. The oldest patients got the most benefit.
DOACs vs. Warfarin: What’s Better for Seniors?
There are two main types of anticoagulants: warfarin and DOACs (direct oral anticoagulants). Here’s how they stack up:| Drug | Stroke Risk Reduction | Bleeding Risk vs. Warfarin | Monitoring Needed? | Reversal Agent Available? |
|---|---|---|---|---|
| Warfarin | ~64% | Baseline | Yes - monthly INR tests | Yes - vitamin K, fresh plasma |
| Apixaban (Eliquis) | 21% better than warfarin | 31% lower major bleeding (in those ≥75) | No | Yes - andexanet alfa |
| Rivaroxaban (Xarelto) | Similar to warfarin | 34% lower intracranial hemorrhage | No | Yes - andexanet alfa |
| Dabigatran (Pradaxa) | 88% better than placebo | Similar to warfarin | No | Yes - idarucizumab |
| Edoxaban (Savaysa) | Comparable to warfarin | 8.5% lower major bleeding | No | Yes - andexanet alfa |
DOACs are now the go-to for most seniors. They don’t need regular blood tests. They’re safer for the brain. And they’re just as effective - even for people over 85. The 2023 FDA approval of andexanet alfa means if someone on rivaroxaban or apixaban has a bad fall and bleeds internally, doctors now have a fast-acting antidote. That wasn’t true a decade ago.
Why So Many Seniors Are Still Not Treated
Despite all this, only about half of eligible seniors take anticoagulants. Why? Because doctors are scared. A 2021 survey found that 68% of primary care doctors would refuse to prescribe a blood thinner to an 85-year-old who’d fallen twice - even if that person had a high stroke risk score (CHA2DS2-VASc = 4).This is a dangerous myth. The American College of Cardiology, American Heart Association, and Heart Rhythm Society all agree: fall history alone is not a reason to avoid anticoagulation. The same goes for age. The 2020 European guidelines say: “Anticoagulation is recommended in all AF patients with CHA2DS2-VASc ≥2, including the very elderly.”
Yet in real life, families report being told to stop the medication. One Reddit thread from 2022 had dozens of caregivers describing how their elderly parent’s doctor refused to renew the prescription after a minor fall. That’s not evidence-based care. That’s fear driving decisions.
How to Stay Safe - Without Stopping the Medicine
You don’t have to choose between stroke and a fall. You can reduce both risks at once. Here’s what works:- Use the HAS-BLED score - it includes fall risk, but doesn’t cancel out anticoagulation. A score above 3 just means you need more monitoring, not less treatment.
- Review all medications - benzodiazepines, sleep aids, opioids, and even some blood pressure drugs can make you dizzy. Cutting those out reduces fall risk more than stopping the blood thinner.
- Fix the home - install grab bars, remove throw rugs, add nightlights. Simple changes cut falls by 30-40%.
- Do the Otago Exercise Program - a 15-minute daily routine of strength and balance exercises shown to reduce falls by 35% in seniors.
- Monitor kidney function - DOACs are cleared by the kidneys. As we age, kidney function drops. Get a simple blood test every 6-12 months. If numbers dip, your doctor can lower the dose.
One study found that when all these steps were taken together, the number of serious falls among seniors on anticoagulants dropped by over 60%. You’re not choosing between safety and treatment. You’re choosing better safety with treatment.
The Numbers Don’t Lie
Let’s put this in real terms. For every 100 octogenarians on anticoagulants for one year:- 24 strokes are prevented
- 3 major bleeds occur
- Net benefit: 21 prevented serious events
That’s not a gamble. That’s a win. And for someone with AFib, the risk of stroke isn’t theoretical - it’s personal. It’s the difference between living independently and needing full-time care. Between speaking clearly and losing your voice. Between being home for Christmas and being in the ICU.
And here’s the hardest truth: if you stop the blood thinner because you’re afraid of falling, you’re not protecting your life - you’re trading one disaster for another.
Should I stop my blood thinner if I’ve fallen before?
No. Having fallen in the past is not a reason to stop anticoagulation. Studies show that the risk of stroke from untreated atrial fibrillation is far greater than the risk of serious bleeding from a fall. Guidelines from major medical societies agree: fall history should not change your treatment plan. Instead, focus on reducing fall risk through home safety, exercise, and medication review.
Are DOACs safer than warfarin for seniors?
Yes, for most seniors. DOACs like apixaban and rivaroxaban have lower rates of brain bleeding and don’t require frequent blood tests. They’re also more predictable. Warfarin works well but needs regular INR checks and is affected by diet and other drugs. DOACs are easier to manage, especially for older adults with complex medication regimens. Apixaban, in particular, has shown the best safety profile in patients over 75.
Can I still take anticoagulants if I have kidney problems?
Yes - but your dose may need adjusting. DOACs are cleared by the kidneys, so if your kidney function drops (creatinine clearance below 50 mL/min), your doctor can reduce the dose. For example, apixaban can be lowered from 5mg to 2.5mg twice daily. Warfarin is not affected by kidney function and may be an option if kidney disease is severe. Regular kidney tests every 6-12 months are essential.
What if I have a fall and start bleeding?
Go to the ER immediately. If you’re on a DOAC, tell them which drug you take - they’ll know what antidote to use. Idarucizumab reverses dabigatran. Andexanet alfa reverses rivaroxaban, apixaban, and edoxaban. These antidotes work in minutes. Even if you’re on warfarin, vitamin K and plasma can be given quickly. Delaying care increases risk - don’t wait to see if it gets better.
Is aspirin enough for stroke prevention in seniors?
No. Aspirin reduces stroke risk by only 22%, while anticoagulants cut it by 60-88%. The BAFTA trial showed that elderly patients on anticoagulants had half the stroke rate of those on aspirin. Aspirin is not a substitute for proper anticoagulation in atrial fibrillation. It’s only used if anticoagulants are truly not an option - and even then, it’s a last resort.

Mike Hammer
February 16, 2026 AT 04:56Man, I’ve seen this so many times. Grandpa falls, docs panic, and suddenly his blood thinner gets yanked. But guess what? He’s still alive because he didn’t have a stroke. That’s the real win. We’re treating fear like it’s a diagnosis.
Esha Pathak
February 18, 2026 AT 03:10Life isn’t a risk-free ride, folks 🌪️. We polish the floors, remove the rugs, and still-someone trips. But denying anticoagulants? That’s like refusing a seatbelt because once you got a scratch on your knee. The math doesn’t lie. Apixaban > Aspirin. Period. 💪
Daniel Dover
February 18, 2026 AT 06:59DOACs are clearly better. No need for INR checks. Less brain bleeds. Easier for seniors. Simple.
Chiruvella Pardha Krishna
February 19, 2026 AT 00:45There is a metaphysical truth here: the fear of death is not death itself. We cling to the illusion of control-removing a blood thinner as if it were a curse. But stroke does not ask permission. It does not wait for consent. It arrives in silence, with the weight of a thousand unspoken goodbyes. The body remembers what the mind refuses to face.
Joe Grushkin
February 19, 2026 AT 09:49Wow. Another article telling old people they’re not allowed to be scared. How noble. Meanwhile, real families are dealing with brain hemorrhages and ER bills. The data looks clean on paper. Real life? Not so neat. And don’t get me started on ‘andexanet alfa’-like that’s just sitting in every ER waiting room.
Betty Kirby
February 20, 2026 AT 23:44Y’all are missing the point. This isn’t about statistics. It’s about dignity. My mom’s doctor told her to stop her meds because she ‘stumbled on the stairs.’ She’s 82. She’s sharp. She’s independent. And now? She’s on aspirin. She’s terrified to walk. She’s not living-she’s surviving. Stop treating seniors like fragile china. They’re not broken just because they fell once.
Kaye Alcaraz
February 22, 2026 AT 05:12Every single recommendation in this post is backed by clinical evidence. The HAS-BLED score includes fall risk, but doesn’t override treatment. The Otago program reduces falls by 35%. DOACs with reversal agents have made treatment safer than ever. This isn’t theory-it’s standard of care. If your provider refuses based on a fall, ask for a second opinion. Your life matters.
Sarah Barrett
February 22, 2026 AT 16:43The data is unequivocal: for patients with CHA2DS2-VASc ≥2, anticoagulation reduces stroke-related mortality by over 60%. The risk of intracranial hemorrhage on DOACs is significantly lower than with warfarin, especially in the elderly. The notion that fall history contraindicates therapy is outdated and unsupported by guidelines. Clinical decision-making must be evidence-based, not fear-based.
Kapil Verma
February 23, 2026 AT 13:48India has 150 million seniors. And we still treat them like burdens. If you’re too scared to give anticoagulants because someone tripped, then maybe you shouldn’t be a doctor. We need courage, not caution. Your grandmother’s life isn’t a liability. It’s a legacy.
Erica Banatao Darilag
February 23, 2026 AT 23:36I just want to say thank you for writing this. My dad was taken off his rivaroxaban after a minor slip on ice. We didn’t know any better. Three months later, he had a mini-stroke. We’re lucky he recovered. But if this post had been around then… we might’ve fought harder. Please keep sharing this. People need to hear it.
Michael Page
February 24, 2026 AT 07:05So… if I’m 88, have AFib, and live alone, I’m supposed to just keep taking DOACs while ignoring that I can’t get up from the couch without help? What’s the plan? Who’s gonna carry me to the ER? The antidote doesn’t fix the fact that I’m falling because I’m weak. You can’t just out-math your frailty.