Combination Therapy: How Combining Medications Improves Outcomes
When we talk about Combination Therapy, the practice of using two or more medicines or treatments together to boost effectiveness or reduce side effects. Also known as combined treatment, it’s a cornerstone of modern health care. Drug Interaction, the way one drug can alter the effect of another when taken together is a key factor doctors assess, because the right mix can amplify benefits while the wrong mix can cause trouble. Another related idea is Polypharmacy, the use of multiple medications by a patient, often seen in chronic disease management. Together, these concepts form a web: combination therapy encompasses drug interaction, it requires dosage optimization, and polypharmacy influences safety monitoring. Understanding this web helps patients and clinicians choose the right partners for their medicines.
Why Combine? The Real Benefits and Risks
Combination Therapy isn’t just a buzzword; it’s a strategic approach. By pairing a cholesterol‑lowering statin with vitamin D, for example, patients may see better heart health while fixing a common deficiency. When an antibiotic like doxycycline meets a pregnancy‑sensitive condition, adjusting the regimen can protect the unborn child. The benefits include stronger therapeutic effects, reduced dosing of each individual drug, and the chance to target multiple disease pathways at once – think of adjunct therapy in cancer where chemo meets immunotherapy. But the flip side is real: overlapping side‑effects, unexpected drug‑drug clashes, and the need for tighter lab monitoring. That’s why clinicians often create a dosing schedule that staggers administration times, uses lower doses, or selects drugs with complementary mechanisms. The goal is to maximize synergy and minimize harm.
In practice, the process starts with a clear clinical goal, followed by a review of each medication’s mechanism, half‑life, and metabolism. Tools like electronic prescribing systems flag potential interactions, while pharmacists play a crucial role in adjusting doses. Patients are encouraged to keep an updated medication list, report new symptoms promptly, and attend regular follow‑ups. By staying on top of dose adjustments and monitoring labs, the risks of polypharmacy can be kept in check. Below you’ll find articles that dive into specific drug pairings, safety checklists, and real‑world advice for managing combination regimens across a range of conditions.
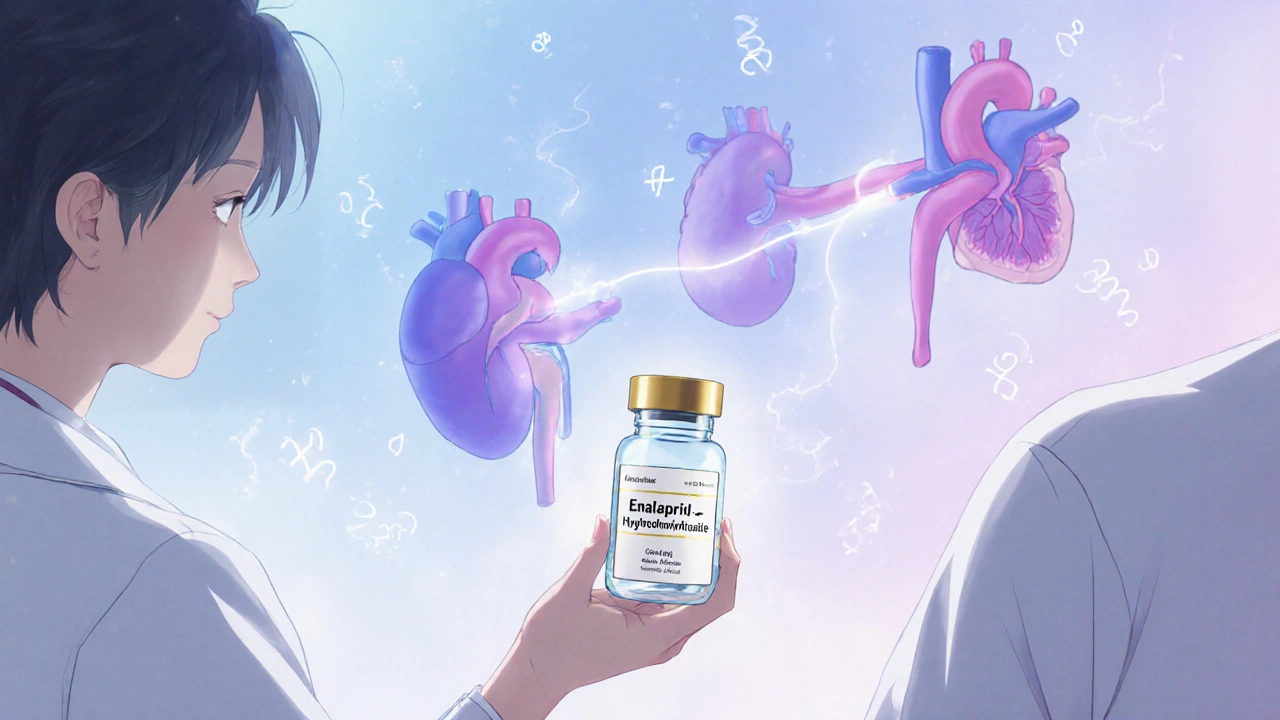
Enalapril‑Hydrochlorothiazide for Hypertension in Chronic Kidney Disease: How It Works and Benefits
Learn how enalapril‑hydrochlorothiazide works, its benefits for hypertension in chronic kidney disease, dosing tips, safety alerts, and real‑world evidence to help clinicians make informed choices.
READ MORE